Actinomycosis and actinobacillosis are two bacterial infections that, despite their similar sounding names, are caused by different organisms and affect the body in diverse ways. These conditions can occur in both humans and animals, leading to various systemic infections that can be serious if not properly treated. Differentiating these diseases is crucial for effective treatment and management.
Actinomycosis is a chronic bacterial infection caused by Actinomyces species, typically manifesting with abscess formation, swelling, and invasive growths that can affect the mouth, lungs, and intestines. Actinobacillosis, on the other hand, is primarily caused by Actinobacillus species, often affecting the mouth, respiratory tract, and skin, and is known for its acute presentation. The distinction between these infections lies in their causative agents, affected areas, and their overall impact on health.
Both conditions require distinct approaches in diagnosis and treatment, emphasizing the need for medical professionals to accurately identify and manage each disease. Early detection and appropriate therapeutic interventions can significantly improve outcomes for affected individuals, highlighting the importance of awareness and understanding among healthcare providers and those at risk.
Basics of Actinomycosis
Definition and Causative Agents
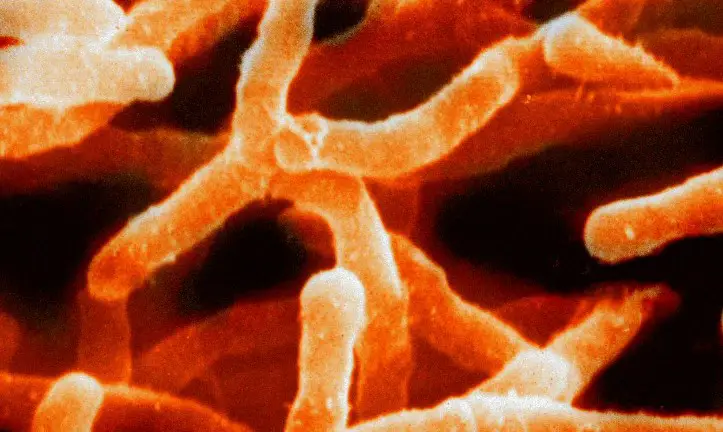
Actinomycosis is a rare type of bacterial infection caused predominantly by the bacterium Actinomyces israelii. These bacteria are part of the normal flora of the mouth and respiratory tract but become pathogenic when they breach the mucosal barrier and invade the body’s tissues. This infection is characterized by its chronic nature and tendency to cause abscesses, typically progressing slowly and capable of causing significant tissue damage.
Common Symptoms
The symptoms of actinomycosis vary depending on the area of the body that is affected:
- Oral Cervicofacial Actinomycosis: This is the most common form, marked by swelling and redness in the jaw, mouth, or neck. Over time, it can cause painful abscesses and open sores that may drain sulfur granules.
- Thoracic Actinomycosis: This form affects the lungs and can mimic symptoms of other respiratory conditions such as cough, chest pain, and fever.
- Abdominal Actinomycosis: In this form, the infection leads to pain, fever, and abdominal swelling. It may also cause weight loss and abdominal masses that can be mistaken for tumors.
- Pelvic Actinomycosis: Often linked with intrauterine devices in women, symptoms include pelvic pain, irregular menstrual bleeding, and signs of a pelvic mass.
Typical Treatment Options
Treatment for actinomycosis typically involves:
- Antibiotics: High doses of penicillin are the mainstay of treatment, often required for a prolonged period ranging from 6 to 12 months to ensure eradication of the infection.
- Surgical Intervention: In cases where abscesses form or significant tissue damage occurs, surgical removal of the affected tissue may be necessary.
- Drainage of Lesions: Draining any abscesses is crucial to relieve discomfort and prevent the spread of the infection.
Basics of Actinobacillosis
Definition and Causative Agents
Actinobacillosis is an infectious disease caused by the bacterium Actinobacillus lignieresii. It primarily affects cattle and other livestock but can also infect humans, particularly those in close contact with affected animals. The disease is characterized by its acute presentation and its potential to cause granulomatous lesions, primarily in the mouth and skin.
Identifying Symptoms
Symptoms of actinobacillosis in animals and humans include:
- Soft Tissue Swelling: Often occurring around the mouth and face in cattle, and can appear in humans typically following an animal bite.
- Wooden Tongue: In cattle, this condition causes a hardening of the tongue, making it difficult for the affected animal to eat and drink.
- Skin Lesions: Granulomatous nodules that may ulcerate are common in both humans and animals.
Available Treatments
The treatment regimen for actinobacillosis involves:
- Targeted Antibiotics: Streptomycin and tetracyclines are commonly used to effectively manage this infection.
- Supportive Care: Ensuring adequate nutrition and hydration is critical, especially in livestock, to maintain health during recovery.
- Surgical Care: Sometimes surgical intervention is needed to remove severely infected tissue.
Key Differences
Pathogens Involved
- Actinomyces species are responsible for actinomycosis.
- Actinobacillus species cause actinobacillosis.
Infection Sites
- Actinomycosis primarily affects the mouth, lungs, and intestines.
- Actinobacillosis mainly targets the mouth, respiratory tract, and skin.
Symptomatology
- Actinomycosis symptoms are often chronic and progressive.
- Actinobacillosis symptoms are generally more acute and localized.
Treatment Protocols
- Actinomycosis requires long-term antibiotic therapy and possible surgical intervention.
- Actinobacillosis treatment might include shorter antibiotic courses and sometimes surgical removal of lesions.
Diagnosis Challenges
Similarities in Symptoms
Both diseases can present with overlapping symptoms such as swelling, abscess formation, and fever, complicating initial clinical assessments.
Diagnostic Techniques
Accurate diagnosis involves:
- Culturing the Bacterium: Essential for confirming the specific type of infection.
- Imaging Studies: Helpful in defining the extent of infection and planning surgical interventions, if needed.
Importance of Accurate Diagnosis
Proper diagnosis is critical as it dictates the specific treatment protocol and significantly affects the prognosis. Misdiagnosis can lead to ineffective treatments and prolonged disease courses.
Impact on Human Health
Epidemiological Data
Actinomycosis and actinobacillosis are relatively rare in humans, but when they occur, they can have significant health impacts. The incidence rate of actinomycosis is estimated at about 1 in 300,000 people annually. Actinobacillosis, being primarily a zoonotic disease, has sporadic human cases, mostly reported in individuals who have direct contact with infected animals.
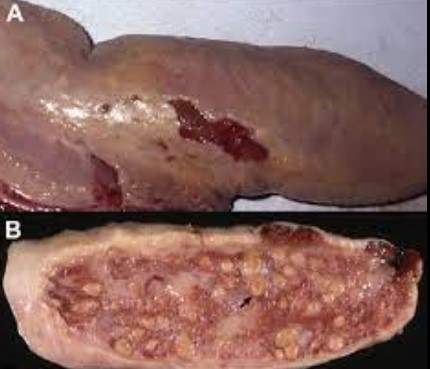
Long-Term Health Effects
The chronic nature of actinomycosis can lead to several long-term health issues if not properly treated. These can include persistent infections, scarring from abscesses, and rare complications such as osteomyelitis (bone infection) when the infection spreads. Actinobacillosis in humans, though generally acute, can cause significant pain and disability if the infection leads to severe granulomatous lesions.
Importance in Public Health
Understanding these diseases is crucial for public health planning, especially in rural and agricultural communities where actinobacillosis is more prevalent. Healthcare providers must be aware of these conditions to ensure early diagnosis and treatment, which can prevent severe outcomes and limit transmission, particularly of actinobacillosis from animals to humans.
Impact on Animal Health
Affects in Livestock
In animals, actinobacillosis primarily affects cattle, causing conditions like wooden tongue, which can severely affect the animal’s ability to eat and maintain weight. Actinomycosis, though less common in livestock compared to humans, can still present as a serious health issue, particularly in swine and cattle, manifesting symptoms similar to those in humans.
Economic Implications
The economic impact of these diseases, particularly actinobacillosis, on livestock production can be considerable. Infected animals may experience:
- Reduced feed intake
- Weight loss
- Decreased milk production
- Lower reproductive performance
These factors contribute to economic losses due to decreased productivity and increased costs for veterinary care.
Management Strategies
Effective management strategies for controlling actinomycosis and actinobacillosis in livestock include:
- Regular veterinary health checks to catch infections early.
- Immediate isolation of infected animals to prevent spread.
- Appropriate antibiotic treatment following veterinary guidance.
Prevention and Control
Preventative Measures
Preventing actinomycosis and actinobacillosis involves a combination of hygiene, animal management, and medical interventions:
- Good Oral Hygiene: In humans, maintaining excellent oral hygiene can help prevent actinomycosis, especially after dental procedures or trauma.
- Safe Handling Practices: People working with livestock should use protective gear and practice good hygiene to reduce the risk of actinobacillosis.
- Regular Veterinary Care: Routine check-ups for livestock can help catch and manage infections early, before they become severe.
Control Strategies in Healthcare
In healthcare settings, controlling these infections includes:
- Awareness and Education: Training healthcare providers to recognize symptoms and risk factors associated with these infections.
- Diagnostic Improvements: Enhancing laboratory capabilities to accurately diagnose these conditions quickly.
- Reporting and Monitoring: Implementing systems for reporting cases to health authorities to monitor and respond to outbreaks effectively.
Recommendations for Livestock Handlers
Livestock handlers can take several steps to minimize the risk of spreading actinobacillosis:
- Regular Inspection of Animals: Monitoring animals for signs of infection and seeking veterinary advice if symptoms appear.
- Hygiene: Washing hands and using disinfectants after handling animals or animal products.
- Quarantine Measures: Isolating new or sick animals from the rest of the herd until they are cleared by a veterinarian.
Frequently Asked Questions
What causes Actinomycosis?
Actinomycosis is caused by Actinomyces israelii, a bacterium that normally lives in the mouth and throat but can cause infection if it breaches mucosal barriers due to injury or other disruptions.
How is Actinobacillosis transmitted?
Actinobacillosis is primarily transmitted through direct contact with contaminated animal products or bites and scratches from infected animals, particularly in agricultural settings.
Can humans get Actinobacillosis from animals?
Yes, humans can contract Actinobacillosis from animals, especially through direct contact with infected livestock, which makes it a zoonotic concern in farming communities.
What are the symptoms of Actinomycosis?
Symptoms of Actinomycosis include painful swelling, abscesses, weight loss, and fever. The infection can also cause sinus tracts that may drain pus.
How are these infections diagnosed?
Both infections are diagnosed using clinical examination, culture of the organism from infected tissues, and imaging studies like X-rays or CT scans to assess the extent of the infection.
Are Actinomycosis and Actinobacillosis treatable?
Yes, both conditions are treatable with antibiotics. Actinomycosis often requires prolonged antibiotic therapy, whereas Actinobacillosis may respond to shorter courses depending on the severity of the infection.
Conclusion
The distinct differences between actinomycosis and actinobacillosis highlight the complexities of bacterial infections that require specific diagnostic and therapeutic strategies. Recognizing and treating these infections effectively depends on a thorough understanding of their pathology, which can prevent potential complications and promote better health outcomes.
By increasing awareness and knowledge about actinomycosis and actinobacillosis, healthcare providers can enhance their diagnostic accuracy and optimize treatment plans. This is essential not only for patient care but also for addressing the broader implications of these diseases in public and animal health.

