Heart disease remains a leading cause of mortality worldwide, compelling medical science to evolve continually in its approach to treatment. Among the advancements, Percutaneous Transluminal Coronary Angioplasty (PTCA) and Percutaneous Coronary Intervention (PCI) have emerged as pivotal procedures in the management of coronary artery disease. These interventions not only promise relief but also offer a glimpse into the future of minimally invasive heart therapies.
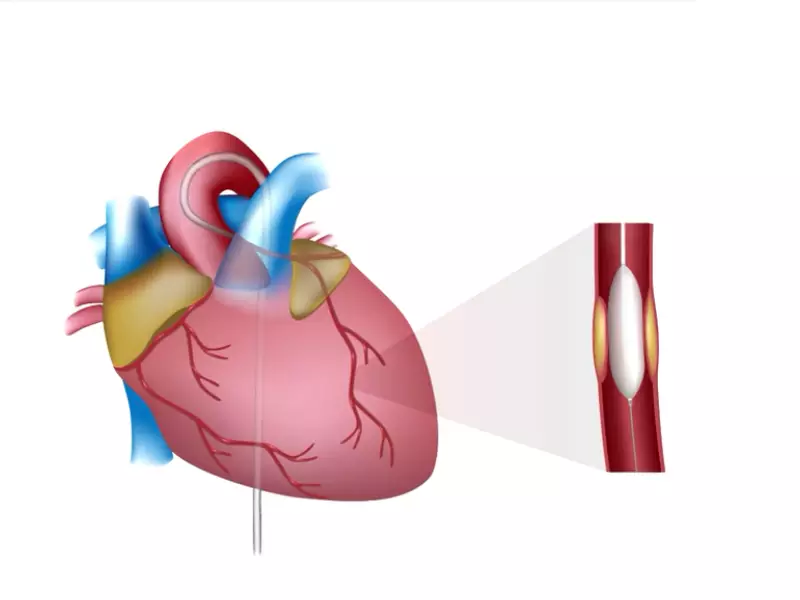
PTCA and PCI are both procedures designed to improve blood flow to the heart muscle in patients with coronary artery disease. PTCA, the original form of coronary angioplasty, involves the use of a balloon catheter to dilate a narrowed artery. PCI encompasses PTCA and may also involve the placement of a stent to keep the artery open. Despite their shared goals, PTCA and PCI differ significantly in approach, technology, and outcomes, making each suited to specific patient needs and conditions.
As heart disease treatment strategies have evolved, so too have the techniques and technologies at the heart of PTCA and PCI. Today, these procedures represent the culmination of decades of research, innovation, and clinical practice, offering hope and healing to those affected by coronary artery disease. Understanding their differences is not just clinically relevant; it’s a testament to the progress in cardiovascular medicine, reflecting on how far we’ve come and where we’re headed in the battle against heart disease.
PTCA Explained
What is PTCA?
Percutaneous Transluminal Coronary Angioplasty (PTCA) is a minimally invasive procedure aimed at improving blood flow to the heart. This technique is used to treat coronary artery disease (CAD), a condition where the arteries supplying blood to the heart muscle become narrowed due to plaque buildup. PTCA helps by widening these arteries, thus enhancing blood flow and reducing heart-related symptoms.
History of PTCA
The evolution of PTCA marks a significant advancement in the treatment of coronary artery disease. Introduced in the late 1970s by Andreas Grüntzig, PTCA has undergone various modifications and improvements. Initially, it was a groundbreaking alternative to coronary artery bypass grafting (CABG), offering a less invasive option for patients. Over the years, the procedure has benefited from technological advancements, including the introduction of stents, which have significantly improved its success rate and reduced the risk of artery re-narrowing.
Procedure of PTCA
Performing a PTCA involves several key steps:
- Patient Preparation: Patients are usually given a sedative to help them relax.
- Accessing the Artery: A catheter is inserted through a small puncture in the arm or groin and guided to the heart’s arteries.
- Locating the Blockage: A special dye is injected through the catheter to visualize the blockage using an X-ray.
- Expanding the Artery: A balloon at the catheter’s tip is inflated at the blockage site, compressing the plaque against the artery walls.
- Stent Placement (if necessary): A stent may be deployed to keep the artery open.
Applications of PTCA
PTCA is recommended for patients experiencing symptoms of coronary artery disease, such as angina (chest pain), especially when medication and lifestyle changes are not effective. It’s also used in urgent situations, like during a heart attack, to quickly open blocked arteries and minimize heart damage.
PCI Unveiled
What is PCI?
Percutaneous Coronary Intervention (PCI) is a broad term that encompasses various procedures, including PTCA, used to treat coronary artery diseases. PCI involves not only the widening of coronary arteries using a balloon but also the placement of stents to keep these arteries open long-term. This method is pivotal in managing acute coronary syndromes and providing symptomatic relief from CAD.
Advances in PCI
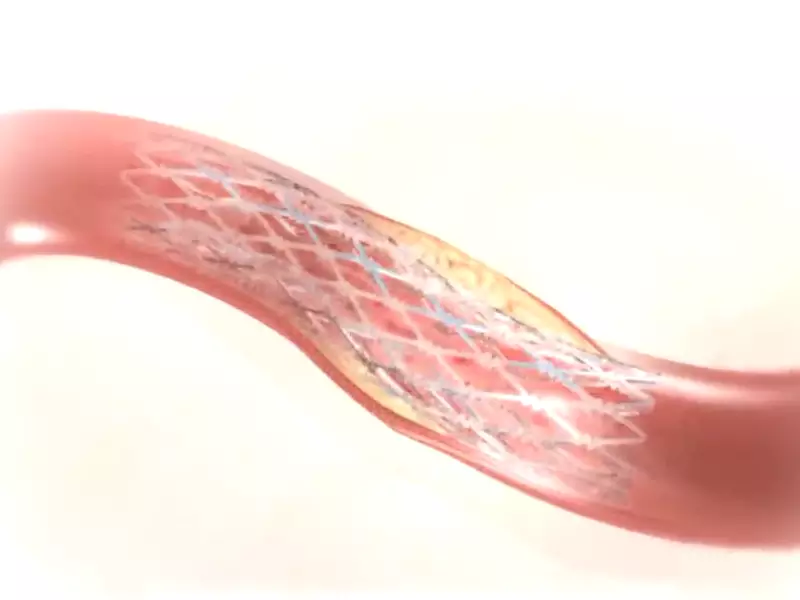
Technological improvements in PCI have been substantial, transforming patient outcomes significantly. Innovations such as drug-eluting stents (DES), which release medication to prevent the artery from getting blocked again, have become a game-changer. Imaging techniques like intravascular ultrasound (IVUS) and optical coherence tomography (OCT) have improved the precision of stent placement, making PCI safer and more effective.
Procedure of PCI
The PCI procedure closely mirrors that of PTCA, with additional steps for stent placement:
- Preparation and Access: Similar to PTCA, with local anesthesia and sedatives.
- Balloon Angioplasty: The balloon expands to open the artery, as in PTCA.
- Stent Deployment: A stent is placed at the dilation site to ensure the artery remains open.
- Post-Procedure Care: Medications may be prescribed to prevent blood clots around the new stent.
Applications of PCI
PCI is recommended for a wider range of coronary artery conditions compared to PTCA alone. It is the treatment of choice for patients with severe CAD, those who have not benefited from medication or lifestyle changes, and for urgent care in acute coronary syndromes. The decision between PTCA and PCI depends on the specific conditions of the artery, patient health, and the presence of comorbidities.
Key Differences Between PTCA and PCI
Technical Aspects
Differences in Procedure Techniques
PTCA and PCI, while often used interchangeably, have distinct procedural differences. PTCA primarily involves balloon angioplasty where a catheter with a small balloon at its tip is used to open up a narrowed artery. On the other hand, PCI is a broader term that includes not only the balloon angioplasty but also the placement of stents to keep the artery open.
Equipment Used
The equipment utilized in PTCA and PCI also highlights their differences. PTCA relies on a balloon catheter. Conversely, PCI uses additional tools, such as stents, which may be bare-metal or drug-eluting, and specialized imaging equipment to guide the placement of these stents more accurately.
Success Rates
Research and clinical trials have consistently shown that PCI has a higher success rate in both the short and long term, primarily due to the use of stents that prevent the artery from narrowing again. This comparative analysis underscores the evolution from PTCA to PCI as a more effective treatment for CAD.
Recovery
Post-procedure Recovery and Care
Recovery and post-care differ subtly between PTCA and PCI. After PTCA, patients may resume normal activities relatively quickly, often within a few days. PCI, involving stent placement, requires a more cautious approach to recovery. Patients are advised to avoid strenuous activities for a longer period and are often prescribed medication to prevent blood clots.
Case Selection
Indications for PTCA
PTCA is typically indicated for patients with a single blockage in a coronary artery and those who have not responded to medication. It’s also used when the blockage is in a location that is easily accessible by the catheter.
Criteria for Choosing PTCA
- Single vessel disease
- Less complex blockages
- Patients with higher surgical risks
Indications for PCI
PCI is recommended for patients with multivessel coronary artery disease, more complex blockages, or those who require immediate intervention, such as during a heart attack.
Criteria for Choosing PCI
- Multivessel disease
- Complex blockages requiring stents
- High risk of restenosis
Risks and Complications
PTCA Risks
Common risks associated with PTCA include artery re-narrowing (restenosis), bleeding at the catheter insertion site, and less commonly, heart attack or stroke during the procedure.
PCI Risks
PCI carries similar risks to PTCA, with the addition of potential stent-related complications, such as stent thrombosis (blood clots forming in the stent) and issues related to long-term stent implantation.
Managing Complications
Strategies for managing these risks include the use of medication to prevent clot formation, careful monitoring of the patient post-procedure, and choosing the most appropriate procedure based on the patient’s health condition and the complexity of the artery disease.
Future Directions
Innovations in PTCA
Upcoming advancements in PTCA focus on enhanced balloon technologies and biodegradable materials that could potentially reduce the risk of restenosis without leaving a permanent implant in the body.
Innovations in PCI
Innovations in PCI are geared towards next-generation stents that are more biocompatible, drug-eluting stents with more effective medication coatings, and improved imaging techniques for more precise stent placement.
Impact on Patient Care
These innovations aim to reduce complications, improve the long-term success of the procedures, and enhance the quality of life for patients with coronary artery disease. As technology advances, treatments are becoming less invasive, recovery times shorter, and outcomes more favorable, marking a significant step forward in the management and care of patients with heart disease.
Frequently Asked Questions
What is PTCA?
PTCA, or Percutaneous Transluminal Coronary Angioplasty, is a minimally invasive procedure used to open up blocked coronary arteries, allowing better blood flow to the heart muscle. It typically involves the insertion of a balloon catheter into the narrowed artery and inflating the balloon at the blockage site to dilate the artery.
How does PCI differ from PTCA?
PCI, or Percutaneous Coronary Intervention, is a broader term that includes PTCA as well as the placement of stents to keep the artery open post-dilation. While PTCA focuses solely on balloon angioplasty, PCI may involve additional techniques to ensure the artery remains open, providing a more permanent solution to coronary artery blockages.
Who is eligible for PTCA or PCI?
Patients with coronary artery disease experiencing symptoms such as chest pain (angina) or those at risk of a heart attack may be considered for PTCA or PCI. The choice between the two depends on the severity of the artery blockage, the number of arteries affected, and overall heart health, assessed by a cardiologist.
What are the risks associated with PTCA and PCI?
Both PTCA and PCI carry risks, including bleeding at the catheter insertion site, blood vessel damage, heart attack, or stroke. However, the risk of serious complications is relatively low and weighed against the benefits of alleviating heart disease symptoms and preventing heart attacks.
Conclusion
The journey through the landscapes of PTCA and PCI reveals the remarkable strides taken in the treatment of coronary artery disease. These procedures, emblematic of the advances in cardiovascular care, not only underscore the progress in medical science but also highlight the nuanced approach required in selecting the right treatment for each patient. As we look to the future, the evolution of PTCA and PCI promises to continue, driven by innovation and the perennial goal of improving patient outcomes.
In choosing between PTCA and PCI, the medical community is guided not just by the technical differences between these procedures but by a commitment to patient-centered care. This commitment ensures that each decision is tailored to the individual’s needs, offering a beacon of hope for those navigating the complexities of heart disease. As we continue to advance, the promise of even more effective treatments looms on the horizon, offering the prospect of longer, healthier lives for those afflicted by coronary artery disease.
