Bacterial infections significantly impact public health worldwide, presenting a challenge in both diagnosis and treatment. Two lesser-known but medically important bacteria are Pasteurella and Haemophilus. Each plays a distinct role in human and animal diseases, and their proper identification is critical for effective medical management.
Pasteurella and Haemophilus are both genera of bacteria that can cause various infections in humans and animals. While they share some similarities, such as their ability to cause respiratory tract infections, they differ significantly in their environmental needs, the severity of the infections they cause, and their treatment protocols. Accurately distinguishing between these two can guide appropriate therapeutic measures and prevent complications.
Pasteurella is typically associated with animal bites and can cause rapid infection at the wound site, leading to severe complications if untreated. On the other hand, Haemophilus predominantly affects the respiratory tracts of children and adults and is known for causing conditions such as pneumonia and meningitis. Understanding their transmission, typical habitats, and impacts on health is essential for clinicians and those at risk of exposure.
Basics of Pasteurella
Definition and Characteristics
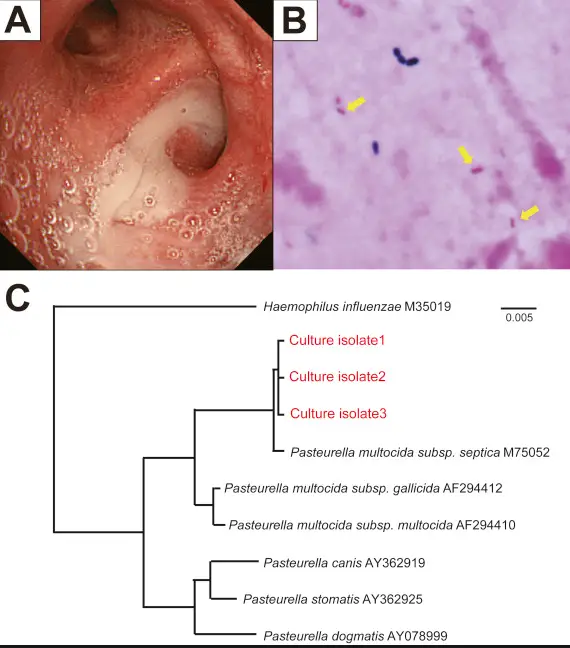
Pasteurella is a genus of bacteria that primarily exists in the mouths of domestic and wild animals but can cause infections in humans following an animal bite or close contact. These organisms are small, non-motile, and often exhibit a bipolar staining pattern under microscopy. They thrive in aerobic environments but can also grow under anaerobic conditions. This adaptability makes Pasteurella a frequent opportunistic pathogen, especially in individuals with compromised immune systems.
Common Strains and Their Impact
Among the various strains of Pasteurella, Pasteurella multocida is the most well-known and clinically significant. It is responsible for a range of infections, from mild skin infections to more severe cases like septicemia and meningitis:
- Skin and soft tissue infections are common following cat or dog bites.
- Respiratory infections may occur, particularly in patients with existing pulmonary diseases.
- Systemic infections such as septicemia can develop in more severe cases, particularly in the elderly or immunocompromised.
Basics of Haemophilus
Definition and Characteristics
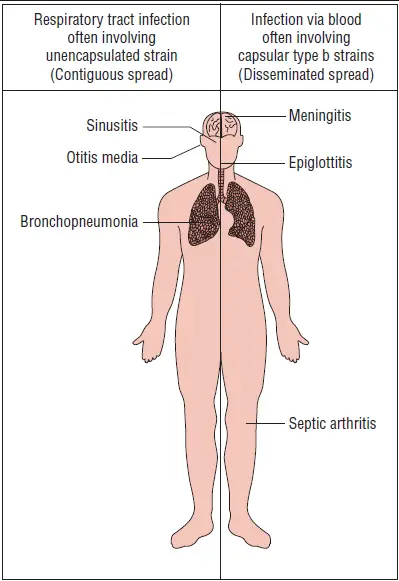
Haemophilus is a genus of Gram-negative bacteria that is known for its requirement of special growth factors present in blood, which classifies them among the haemophili. These bacteria are typically small, rod-shaped, and can be part of the normal respiratory tract flora. However, certain conditions allow Haemophilus to become pathogenic, leading to various infections, primarily affecting the respiratory tract and occasionally more invasive diseases.
Common Strains and Their Impact
Haemophilus influenzae is the most prominent strain, known for its impact on both children and adults. It is differentiated into serotypes based on its capsular polysaccharides, with type b (Hib) being historically the most significant:
- Respiratory infections such as pneumonia and bronchitis are frequent.
- Invasive diseases like meningitis and epiglottitis, primarily caused by Hib, can be life-threatening without proper vaccination and treatment.
- Otitis media is commonly seen in children as a result of Haemophilus infections.
Comparative Analysis
Structural Differences
While both Pasteurella and Haemophilus are small, Gram-negative bacteria, their structural compositions show significant differences:
- Cell wall structure: Pasteurella has a thinner peptidoglycan layer compared to Haemophilus, affecting its susceptibility to certain antibiotics.
- Capsular material: Haemophilus strains, especially Hib, have a robust capsule that is a major virulence factor, unlike most Pasteurella strains.
Genetic Differences
The genetic content of these bacteria highlights their adaptive strategies and pathogenic potentials:
- Genome size: Haemophilus genomes are generally smaller than those of Pasteurella, which reflects their streamlined metabolic requirements adapted to life within the human host.
- Virulence genes: Both genera have evolved specific virulence factors, but Haemophilus tends to have more specialized adaptations for survival in the human respiratory tract.
Infection Mechanisms
How Pasteurella Infects
Pasteurella typically enters the human body through wound infections following an animal bite:
- The bacteria are introduced directly into the tissue, where they multiply rapidly.
- Enzymes and toxins produced by the bacteria help spread the infection by breaking down tissues and evading the immune response.
How Haemophilus Infects
Haemophilus primarily infects through respiratory droplets:
- The bacteria colonize the mucosal surfaces of the upper respiratory tract.
- From there, they can invade deeper respiratory tissues or bypass the mucosal barrier to cause systemic infections.
Clinical Symptoms
Symptoms of Pasteurella Infections
Symptoms following a Pasteurella infection can arise quickly and include:
- Pain and swelling at the infection site
- Redness and warmth around the wound
- In more severe cases, fever and signs of systemic infection may develop.
Symptoms of Haemophilus Infections
Haemophilus infections present a variety of symptoms based on the infection site:
- Respiratory symptoms like coughing and difficulty breathing
- Fever and fatigue in more systemic cases
- In children, symptoms of ear infections or stiff neck in meningitis
Diagnostic Approaches
Tests for Pasteurella
Diagnosing Pasteurella infections generally involves culture and sensitivity tests. Here’s a step-by-step guide on how clinicians typically approach testing:
- Sample Collection: Direct samples from the wound or site of infection are collected.
- Culture: The specimen is cultured in a laboratory to identify the growth of Pasteurella species.
- Microscopy: Gram staining and microscopic analysis help confirm the presence of Pasteurella.
- Sensitivity Testing: Determines the most effective antibiotics for treatment.
Advanced molecular techniques such as PCR (polymerase chain reaction) may also be employed for more rapid and precise identification.
Tests for Haemophilus
Identifying Haemophilus, particularly H. influenzae, involves several key diagnostic steps:
- Specimen Collection: Samples are typically taken from the throat, sputum, or other respiratory secretions.
- Culture: Culturing on chocolate agar, which provides the necessary growth factors.
- Serotyping: To determine the specific type (e.g., Hib), which is crucial for epidemiological tracking and treatment decisions.
- Molecular Diagnostics: PCR and other DNA-based tests offer a quick and accurate method to identify Haemophilus strains.
Treatment Strategies
Treating Pasteurella Infections
Treatment for Pasteurella infections is straightforward but must be prompt to prevent complications:
- Antibiotics: Effective antibiotics include penicillin, tetracycline, and cephalosporins. Treatment duration may vary based on the infection severity.
- Wound Care: Proper cleaning and care of any bite wounds are crucial to prevent further infection.
Treating Haemophilus Infections
Haemophilus infections require targeted therapies, particularly for invasive diseases:
- Antibiotics: A broad spectrum of antibiotics such as ampicillin, with or without beta-lactamase inhibitors, is commonly used.
- Supportive Care: For severe cases like meningitis, supportive care in a hospital setting is necessary.
Prevention Techniques
Vaccination and Public Health
Vaccination is the cornerstone of preventing severe Haemophilus influenzae type b infections:
- Hib Vaccine: Widely administered in childhood immunization programs to prevent meningitis, pneumonia, and other severe diseases.
- Public Health Campaigns: Educating the public about the importance of vaccination and maintaining high immunization rates is crucial for controlling outbreaks.
Lifestyle and Environmental Factors
Environmental and lifestyle changes can also help reduce the risk of bacterial infections:
- Hygiene: Regular handwashing and wound care can significantly decrease the risk of infection.
- Animal Handling: Proper handling and training of pets can reduce the risk of bites and scratches that could lead to Pasteurella infections.
Impact on Public Health
Epidemiology of Pasteurella
Pasteurella is most commonly associated with animal bites and scratches:
- Incidence: It is estimated that up to 50% of cat bite wounds culture positive for Pasteurella.
- Risk Groups: Individuals with close contact with animals, such as veterinarians and pet owners, are at higher risk.
Epidemiology of Haemophilus
Haemophilus influenzae, especially non-b type strains, remain a significant cause of respiratory infections:
- Global Impact: Despite vaccination efforts, there are still many cases of Haemophilus-related respiratory infections annually.
- Risk Populations: Children under five and elderly individuals are particularly susceptible.
Future Research Directions
Current Research on Pasteurella
Research on Pasteurella focuses on developing better diagnostic tools and understanding antibiotic resistance patterns:
- Genomic Studies: These aim to map out resistance genes and potentially develop targeted therapies.
- Vaccine Development: There is ongoing research into creating vaccines for more comprehensive protection against various Pasteurella strains.
Current Research on Haemophilus
For Haemophilus, the research aims to improve existing vaccines and treatment approaches:
- Vaccine Enhancement: Efforts are being made to develop vaccines that cover more strains, especially for non-b type Haemophilus.
- Pathogenesis Understanding: Studying how Haemophilus infects and evades the immune system can lead to better therapeutic strategies.
FAQs
What is Pasteurella?
Pasteurella is a genus of bacteria commonly found in the mouths of animals, including cats and dogs. It can cause infections in humans primarily through animal bites or close contact with pets. The infections may manifest as skin and soft tissue infections, and in more severe cases, can lead to systemic illnesses.
How does Haemophilus infect humans?
Haemophilus primarily infects humans through respiratory droplets. This bacterium can cause a range of infections, particularly in children, including otitis media, bronchitis, and invasive diseases like meningitis and bloodstream infections. The pathogen is adapted to invade the mucosal surfaces of the respiratory tract.
Can you vaccinate against Haemophilus infections?
Yes, vaccination is available and effective against certain strains of Haemophilus influenzae, particularly type b (Hib). The Hib vaccine is part of routine pediatric immunization schedules and significantly reduces the risk of severe diseases such as pneumonia and meningitis caused by this bacterium.
Are Pasteurella infections treatable?
Pasteurella infections are typically treatable with antibiotics. Prompt medical attention is crucial, especially following an animal bite, to prevent the infection from worsening. Treatment usually involves cleaning the wound and antibiotic therapy to combat the bacteria effectively.
Conclusion
In concluding, Pasteurella and Haemophilus represent two distinct challenges in the realm of bacterial infections, each necessitating specific clinical awareness for accurate diagnosis and treatment. Recognizing the differences between these pathogens is crucial for implementing the right treatment strategies and preventive measures, ultimately reducing their impact on public health.
The importance of education and awareness cannot be overstated, as both play vital roles in preventing the spread of these infections. Whether through vaccination or understanding the risks associated with animal bites, knowledge empowers individuals to take proactive steps in protecting their health against these bacterial threats.

