Blood types are a crucial element of human biology that influence health, medical treatments, and transfusions. Each blood type, determined by the presence or absence of certain antigens, plays a vital role in our body’s immune response and compatibility with donated blood. Among these, O positive and O negative blood types are particularly significant due to their unique characteristics and compatibility profiles.
The primary difference between O positive and O negative blood types lies in the presence of the Rh factor: O positive blood has the Rh factor, while O negative blood does not. This distinction makes O negative blood universally compatible with all recipients in emergency situations, whereas O positive blood, being the most common blood type, is highly versatile but not universally compatible.
Understanding the nuances of O positive and O negative blood types is more than academic curiosity—it’s a matter of life-saving importance. These blood types not only dictate who can donate to whom but also have implications for medical procedures, pregnancies, and managing emergency situations where blood transfusions are required. By exploring these aspects, we can appreciate the critical role that blood type compatibility plays in healthcare and emergency medical services.

Blood Basics
Blood Type Fundamentals
Blood types are a crucial aspect of our health and medical treatments. Essentially, a blood type is a classification of blood based on the presence or absence of antibodies and inherited antigenic substances on the surface of red blood cells. These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system.
The significance of blood types extends far beyond the laboratory. In medical settings, they are pivotal for safe blood transfusions, organ transplants, and in managing pregnancy. Matching blood types between donors and recipients reduces the risk of adverse reactions, making understanding blood types a matter of life-saving importance.
The ABO System
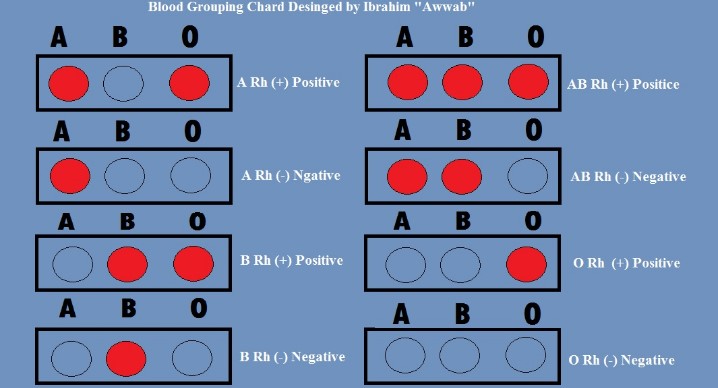
The ABO blood group system is the most recognized and critical for blood transfusions. It categorizes blood into four main types: A, B, AB, and O, based on the type of antigens present on the surface of the red blood cells. Understanding these types helps in identifying compatible blood for transfusions.
- Type A has A antigens.
- Type B has B antigens.
- Type AB has both A and B antigens, making it a universal recipient.
- Type O lacks these antigens, but has both A and B antibodies, making it a universal donor for red blood cells.
Rh Factor
The Rh factor adds another layer to blood typing, indicating the presence (+) or absence (-) of the RhD antigen on the red blood cells. This detail is crucial, especially in pregnancy, where an Rh-negative mother carrying an Rh-positive fetus can develop antibodies against the fetus’s red blood cells, leading to complications.
The Rh factor’s significance extends to blood transfusions and organ transplants, necessitating matching Rh types to prevent immune reactions. An Rh-negative individual receiving Rh-positive blood can develop an immune response, making the accurate determination of the Rh factor vital in medical care.
O Positive Blood Type
Overview
O positive is the most common blood type, found in about 37.4% of the world’s population. Its prevalence makes it extremely important in the context of blood donations and transfusions.
Prevalence and Characteristics
O positive blood is characterized by the absence of A and B antigens on the red blood cells but has the RhD antigen, making it Rh positive. This blood type plays a critical role in the blood supply chain, especially in emergency transfusions and for patients with O positive blood.
Compatibility for Donations and Transfusions
O positive blood can be donated to individuals with O positive, A positive, B positive, and AB positive blood types, covering a significant portion of the population. However, individuals with O positive blood can only receive O positive and O negative blood, limiting their donor pool.
Advantages
- Universal donor for Rh-positive patients: O positive blood can be used in transfusions for any Rh-positive patient, making it highly valuable.
- Prevalence: Its commonality ensures a relatively steady supply for transfusions.
Considerations
- Receiving blood: Limitations exist for O positive individuals in receiving blood, primarily restricted to O types.
- Pregnancy: The Rh factor can complicate pregnancies, necessitating careful management to prevent Rh incompatibility issues.
O Negative Blood Type
Overview
O negative blood type is known for its rarity and unique ability to be a universal donor for red blood cells, making it incredibly valuable in emergency situations and for patients with rare blood types.
Rarity and Unique Properties
Representing only about 6.6% of the population, O negative blood lacks both A and B antigens and the RhD antigen. This absence makes it safe for transfusing to nearly any patient, a property no other blood type possesses.
Advantages
- Emergency transfusion capabilities: O negative blood is the go-to choice in emergency situations where the patient’s blood type is unknown.
- Critical role in medical emergencies: Its universality ensures that it is always in high demand at hospitals and blood banks.
Considerations
- Finding compatible donors: For O negative individuals, only O negative blood is fully compatible, posing challenges in finding suitable donors.
- Pregnancy: O negative women can face complications if carrying an Rh-positive child, requiring careful monitoring and management.

Compatibility and Transfusion
Transfusion Basics
Blood transfusions are a critical component of modern healthcare, saving millions of lives each year. The success of a transfusion largely depends on compatibility between the donor’s and recipient’s blood types. Compatibility prevents the recipient’s immune system from attacking the transfused blood, which can cause serious complications.
- ABO and Rh systems are the main factors considered to ensure compatibility.
- Cross-matching tests are performed before transfusions to confirm compatibility and prevent adverse reactions.
Understanding and matching both the ABO blood type and the Rh factor are crucial steps to ensure the safety and effectiveness of blood transfusions.
O Positive vs. O Negative
Detailed Comparison in Transfusions
When comparing O positive and O negative blood types in the context of transfusions, several key differences emerge:
- O positive blood can be given to any Rh-positive patient regardless of their ABO blood type. This makes O positive blood extremely valuable, especially since it is the most common blood type.
- O negative blood, on the other hand, is a universal donor for all ABO and Rh blood types. It is especially critical in emergency situations where the patient’s blood type might not be immediately known.
Implications for Blood Banks and Emergency Situations
- Emergency Readiness: O negative blood is the go-to choice for emergency transfusions. Its universal compatibility means it can be given to anyone in critical situations, making it a vital resource in emergencies.
- Blood Banks: The high demand for O negative blood puts pressure on blood banks to maintain a sufficient supply. Despite its rarity, efforts are continually made to encourage donations of this blood type.
Health Implications
Medical Procedures
The compatibility of blood types is not only important in transfusions but also plays a significant role in surgeries and medical treatments, including organ transplants. Matching the donor’s and recipient’s blood types reduces the risk of rejection and other complications.
Pregnancy and Childbirth
The Rh factor is particularly significant in pregnancy. An Rh-negative mother carrying an Rh-positive child can develop antibodies against the baby’s blood, a condition known as Rh incompatibility. This can lead to serious health issues for the unborn child, including anemia, jaundice, and heart failure.
- Managing Rh Incompatibility: Pregnant women are tested for their Rh factor early in pregnancy. If there is a risk of Rh incompatibility, doctors can administer Rh immune globulin to prevent the mother from producing antibodies against her baby’s blood cells.
Myths vs. Facts
Common Misconceptions
Several myths surround blood donation and blood types, often deterring individuals from donating. For instance, some believe that certain blood types should avoid certain foods or that blood type affects personality. These beliefs lack scientific backing and should not influence decisions regarding blood donation or diet.
Facts About Blood Type Diet and Personality Traits
Research has debunked the myth that blood type diets offer health benefits or that a person’s blood type can determine their personality traits. The most important fact to remember is the critical role of blood donation in saving lives, irrespective of myths and misconceptions.
Global Impact
Blood Type Distribution
The distribution of blood types varies globally, with O positive being the most common and O negative much rarer. Understanding this distribution helps in planning and executing blood donation drives and in setting policies to encourage donations of rarer blood types.
Influence on Blood Donation Drives and Policies
Countries and regions adapt their blood donation drives and policies according to the prevalence of different blood types in their populations. For instance, areas with higher rates of O negative populations might have more targeted campaigns to encourage donations from these individuals.
Challenges in Healthcare
Supply and Demand for O Negative Blood
The universal donor status of O negative blood means it is in high demand, especially for emergency transfusions. However, its rarity poses a challenge in maintaining an adequate supply.
Strategies to Manage Shortages
Blood banks and health organizations employ several strategies to manage shortages of O negative blood, including:
- Encouraging regular donations from individuals with O negative blood.
- Educating the public about the importance of blood donation.
- Optimizing the use of O negative blood to ensure it is available for emergencies.
Frequently Asked Questions
What makes O negative blood unique?
O negative blood is considered unique due to its universal donor status. It lacks the A, B, and Rh antigens, making it safe to transfuse into patients of any blood type in urgent situations. This universality is crucial in emergency medical settings, where there may not be time to determine a patient’s blood type.
Can O positive receive O negative blood?
Yes, individuals with O positive blood can receive O negative blood. O negative is compatible with all blood types due to its lack of A, B, and Rh antigens. However, it’s typically reserved for emergency situations to preserve the rare O negative supply for when it’s most needed.
How does blood type affect pregnancy?
Blood type can significantly impact pregnancy due to the Rh factor. If an Rh-negative mother is pregnant with an Rh-positive baby, it may lead to Rh incompatibility, where the mother’s immune system attacks the baby’s red blood cells. Proper prenatal care includes blood type testing to manage and prevent complications from Rh incompatibility.
Why is blood type important in transfusions?
Blood type is critical in transfusions to prevent adverse reactions. Transfusing blood with incompatible antigens can trigger an immune response, leading to dangerous complications. Understanding blood types ensures that patients receive compatible blood, maximizing the safety and effectiveness of transfusions.
Conclusion
The distinctions between O positive and O negative blood types are more than mere labels; they are essential knowledge that underpins safe medical practices, from transfusions to managing pregnancies. Recognizing these differences helps ensure that each patient receives the most compatible blood in both routine and emergency scenarios, significantly reducing the risk of complications.
As we continue to navigate the complexities of blood type compatibility, it’s clear that the value of understanding and managing these differences cannot be overstated. Whether for an individual assessing their donation options or a medical professional preparing for a procedure, the knowledge of O positive and O negative blood types remains a cornerstone of modern medicine, emphasizing the importance of targeted and informed healthcare strategies.