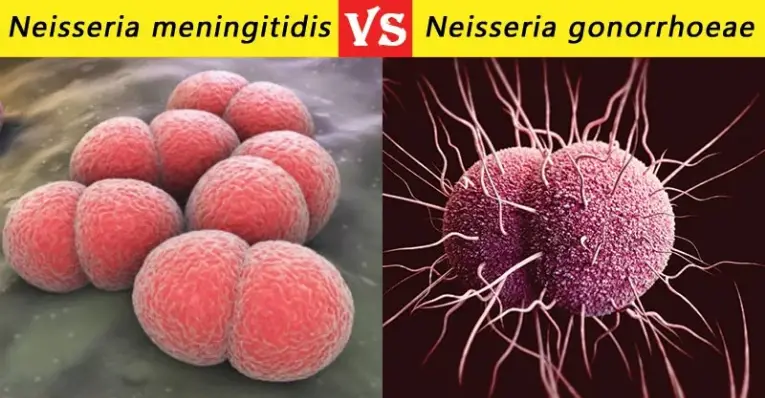
Neisseria gonorrhoeae and Neisseria meningitidis are two closely related bacteria notorious for their impact on human health. Both organisms belong to the genus Neisseria and share many genetic and biological features, yet they cause distinctly different diseases. Each has adapted uniquely to its human host, manifesting different symptoms and challenges in diagnosis and treatment.
Neisseria gonorrhoeae primarily causes gonorrhea, a common sexually transmitted infection characterized by discharge and painful urination. On the other hand, Neisseria meningitidis is the leading cause of bacterial meningitis, leading to inflammation of the brain and spinal cord membranes, often marked by stiff neck, fever, and headache. These differences highlight the importance of accurate diagnosis and targeted treatment.
This discussion aims to clarify the distinctions and similarities between these two bacteria, focusing on their transmission methods, infection mechanisms, and the health challenges they pose. Understanding these factors is crucial for developing effective prevention and treatment strategies, contributing to better public health outcomes.
Characteristics Overview
Neisseria Gonorrhoeae
Basic Description
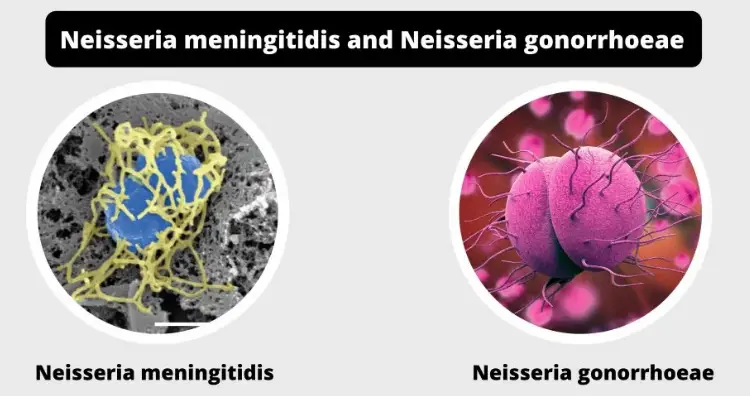
Neisseria gonorrhoeae, often simply referred to as gonococcus, is a gram-negative diplococcus bacterium. It is exclusively pathogenic to humans and is known for causing gonorrhea, a highly contagious sexually transmitted disease. The bacteria’s shape allows it to nestle into the mucous membranes of the human body, where it can evade the host’s immune defenses more effectively.
Habitat and Transmission
Neisseria gonorrhoeae thrives in the warm, moist areas of the reproductive tract, including the cervix, uterus, and fallopian tubes in women, and in the urethra in both men and women. It can also infect the mucous membranes of the mouth, throat, eyes, and anus. Transmission occurs primarily through sexual contact with an infected partner, including vaginal, anal, and oral sex. The high rate of asymptomatic cases complicates efforts to control its spread, as many individuals may not know they are infected.
Neisseria Meningitidis
Basic Description
Neisseria meningitidis, also known as meningococcus, is another gram-negative bacterium that differs significantly from gonococcus in its impact and manifestation. It is the leading cause of bacterial meningitis in children and young adults worldwide. Meningococcus is noted for its ability to cause rapid and severe infections, leading to serious conditions such as meningitis and septicemia.
Habitat and Transmission
This bacterium colonizes the nasopharynx, a part of the pharynx that covers the back of the nose and throat. While it is a common inhabitant of this region in a sizable percentage of the population, it rarely leads to illness. Transmission of Neisseria meningitidis is through droplets from respiratory and throat secretions of infected persons. Close contact or living in close quarters can facilitate the spread of the disease, making outbreaks possible in settings like schools and dormitories.
Infection Mechanisms
Neisseria Gonorrhoeae
Pathogenic Traits
Neisseria gonorrhoeae has several virulence factors that enable it to attach to host cells, evade the immune system, and cause disease. These include pili, which help in attachment to cells, and outer membrane proteins that protect against immune system attacks. The bacteria can also alter its surface proteins to avoid detection, making it a challenging pathogen to target.
Infection Process
The infection process begins when the bacteria attach to the mucous membranes of a new host. From there, they multiply and spread, causing inflammation and the typical symptoms of gonorrhea. The ability of Neisseria gonorrhoeae to resist phagocytosis allows it to persist in the host and spread to new individuals.
Neisseria Meningitidis
Pathogenic Traits
Neisseria meningitidis is equipped with capsules that help it avoid phagocytosis. It also has pili for attachment to cells and iron-acquisition mechanisms that allow it to thrive in the hostile environment of the host’s body. These traits make it a formidable pathogen capable of causing swift and severe infections.
Infection Process
The infection by Neisseria meningitidis starts when it breaches the mucosal barrier of the nasopharynx. Once in the bloodstream, it can reach the meninges and other vital organs. The rapid multiplication of the bacteria leads to the release of endotoxins, which trigger severe inflammation and symptoms associated with meningitis and septicemia.
Clinical Manifestations
Neisseria Gonorrhoeae
Symptoms and Complications
The primary symptoms of gonorrhea include painful urination, abnormal discharge from the penis or vagina, and, in women, possible pelvic pain. If untreated, it can lead to complications such as pelvic inflammatory disease in women and epididymitis in men, which can result in infertility.
Target Populations
Gonorrhea predominantly affects sexually active teenagers and young adults. High-risk behaviors, multiple sexual partners, and lack of condom use increase the risk of transmission and infection.
Neisseria Meningitidis
Symptoms and Complications
Meningitis caused by Neisseria meningitidis is characterized by sudden onset of fever, headache, and a stiff neck, often accompanied by nausea, vomiting, photophobia (sensitivity to light), and altered mental status. Septicemia can result in a rapid and severe progression, often leading to fatal outcomes if not treated promptly.
Target Populations
Infants, teenagers, and young adults are the most susceptible to meningococcal disease. Living in close quarters, such as dormitories or military barracks, also increases the risk of outbreaks among these groups.
Diagnostic Approaches
Neisseria Gonorrhoeae
Laboratory Tests
For diagnosing gonorrhea, several types of laboratory tests are available:
- Nucleic Acid Amplification Tests (NAATs): These are the most sensitive tests for detecting Neisseria gonorrhoeae and are considered the gold standard. NAATs can identify the genetic material of the bacteria in urine samples or swabs from the affected area.
- Culture: This method involves growing the bacteria on a culture medium, which is then tested to confirm the presence of Neisseria gonorrhoeae. It is useful for testing antibiotic susceptibility.
- Gram Stain: A quick test primarily used for symptomatic men, where a sample from the urethra is stained and examined under a microscope for the presence of gram-negative diplococci.
Diagnostic Criteria
Diagnosis of gonorrhea requires both clinical evaluation and confirmatory laboratory tests. The criteria include identifying typical symptoms along with a positive test result from any of the following:
- A positive NAAT from a sample of the affected area.
- A culture that shows the growth of Neisseria gonorrhoeae.
- For men, a gram stain showing gram-negative diplococci directly from a urethral sample.
Neisseria Meningitidis
Laboratory Tests
Effective laboratory tests to diagnose infections caused by Neisseria meningitidis include:
- Polymerase Chain Reaction (PCR): Highly sensitive in identifying the DNA of Neisseria meningitidis in blood or cerebrospinal fluid (CSF).
- Culture: Growing the bacteria from samples of blood or CSF is crucial, particularly for determining antibiotic sensitivity.
- Latex Agglutination Test: Used on CSF to detect the presence of meningococcal antigens.
Diagnostic Criteria
The diagnosis of meningococcal disease involves clinical signs of meningitis or septicemia and is confirmed by:
- A positive PCR test or culture from blood or CSF.
- Detection of antigens in CSF using latex agglutination, although this test is less commonly used now due to its lower sensitivity compared to PCR.
Treatment Strategies
Neisseria Gonorrhoeae
Antibiotic Choices
The treatment of gonorrhea primarily involves antibiotics, with current guidelines recommending:
- Ceftriaxone: An extended-spectrum cephalosporin administered intramuscularly.
- Azithromycin or Doxycycline: Often given along with ceftriaxone to cover potential co-infection with Chlamydia trachomatis.
Resistance Issues
Antibiotic resistance in Neisseria gonorrhoeae has become a significant concern:
- Strains resistant to fluoroquinolones and older antibiotics are widespread.
- Emerging resistance to cephalosporins and azithromycin complicates treatment choices, necessitating ongoing surveillance and adaptation of treatment guidelines.
Neisseria Meningitidis
Antibiotic Choices
Treatment for meningococcal disease must be started immediately and usually includes:
- Penicillin or Ceftriaxone: These antibiotics are effective for most cases of meningococcal meningitis and septicemia.
- Rifampin, Ciprofloxacin, or Ceftriaxone for prophylactic treatment of close contacts.
Resistance Issues
While less common than in gonococci, resistance in Neisseria meningitidis, particularly to penicillin, has been noted. Monitoring and susceptibility testing are critical for guiding appropriate antibiotic use.
Prevention and Control
Neisseria Gonorrhoeae
Vaccines and Research
Currently, there are no vaccines available to prevent gonorrhea. Research is ongoing to develop a vaccine that can effectively prevent infection by targeting the bacteria’s unique mechanisms of infection and survival.
Public Health Strategies
Public health strategies to control gonorrhea include:
- Routine Screening: Recommended for sexually active individuals, especially those at high risk.
- Education and Awareness: Programs aimed at educating the public about safe sex practices and the importance of regular testing.
Neisseria Meningitidis
Vaccines and Research
Vaccines against Neisseria meningitidis are highly effective and available for different age groups. These include:
- Conjugate Vaccines: Protect against several common serogroups of meningococcus.
- Polysaccharide Vaccines: Older vaccines that cover multiple serogroups but are less effective in young children.
Public Health Strategies
Strategies to prevent meningococcal disease include:
- Mass Vaccination Campaigns: Especially in areas with frequent outbreaks.
- Prophylactic Antibiotics: For close contacts of infected individuals to prevent secondary cases.
Epidemiological Data
Incidence and Prevalence
Both diseases have significant global impacts but vary greatly by region and population:
- Gonorrhea is one of the most common sexually transmitted infections worldwide, with millions of new cases each year.
- Meningococcal disease is less common but has a higher potential for large outbreaks, particularly in the “meningitis belt” of sub-Saharan Africa.
Global Impact Comparisons
The global impact of these diseases underscores the need for effective prevention and control measures:
- Gonorrhea contributes significantly to reproductive health issues, including infertility and ectopic pregnancies.
- Meningococcal disease, although less frequent, can cause rapid and severe outbreaks, leading to high morbidity and mortality in affected populations.
Frequently Asked Questions
What is Neisseria gonorrhoeae?
Neisseria gonorrhoeae is a bacterium that causes gonorrhea, a sexually transmitted disease. It infects the mucous membranes of the reproductive tract, as well as the mouth, throat, eyes, and anus.
How is Neisseria meningitidis transmitted?
Neisseria meningitidis is primarily spread through respiratory and throat secretions (saliva or spit). It can lead to meningitis and other severe infections and is particularly dangerous in crowded conditions or close communities.
What are the symptoms of gonorrhea?
Symptoms of gonorrhea include painful urination, pus-like discharge from the penis or vagina, and, occasionally, painful or swollen testicles. Women may also experience increased vaginal discharge and pelvic pain.
How can meningococcal disease be prevented?
Meningococcal disease can be prevented through vaccination, which is recommended for people in high-risk groups or those who might be exposed to the disease through travel or community outbreaks.
Can Neisseria infections be treated with antibiotics?
Yes, both gonorrhea and meningococcal disease can be treated with antibiotics. However, resistance to common antibiotics is increasing, making it crucial to use them appropriately and continue searching for new treatment options.
Conclusion
As Neisseria gonorrhoeae and Neisseria meningitidis continue to pose significant health challenges worldwide, understanding their differences is not merely academic but a critical aspect of clinical practice. Recognizing the distinct pathologies and transmission vectors of these bacteria aids in the swift and accurate diagnosis necessary for effective treatment.
The ongoing research and development of vaccines and new antibiotics are vital in combating the resistance issues that both bacteria present. By staying informed about the latest advances and recommendations, health professionals and the public can better prevent and manage these potentially devastating infections.

