Bacterial pneumonia is a significant health concern that can stem from various pathogens, with Klebsiella pneumoniae and Streptococcus pneumoniae being two prominent culprits. Both bacteria lead to serious respiratory conditions, yet they present with different characteristics and implications for treatment. It is essential to differentiate between these pathogens to manage the disease effectively.
Klebsiella pneumoniae and Streptococcus pneumoniae are different types of bacteria causing pneumonia, with distinct modes of infection, symptoms, and treatment approaches. Klebsiella pneumoniae often affects individuals with compromised immune systems and is known for its antibiotic resistance, while Streptococcus pneumoniae is more common in the community and can be prevented through vaccination.
While both bacteria cause lung infections, their impact varies significantly across different populations and healthcare settings. Recognizing the differences in their pathological presentation and the resulting clinical implications is crucial for effective treatment and prevention strategies.
Bacterial Profiles
Klebsiella Pneumoniae
General Characteristics
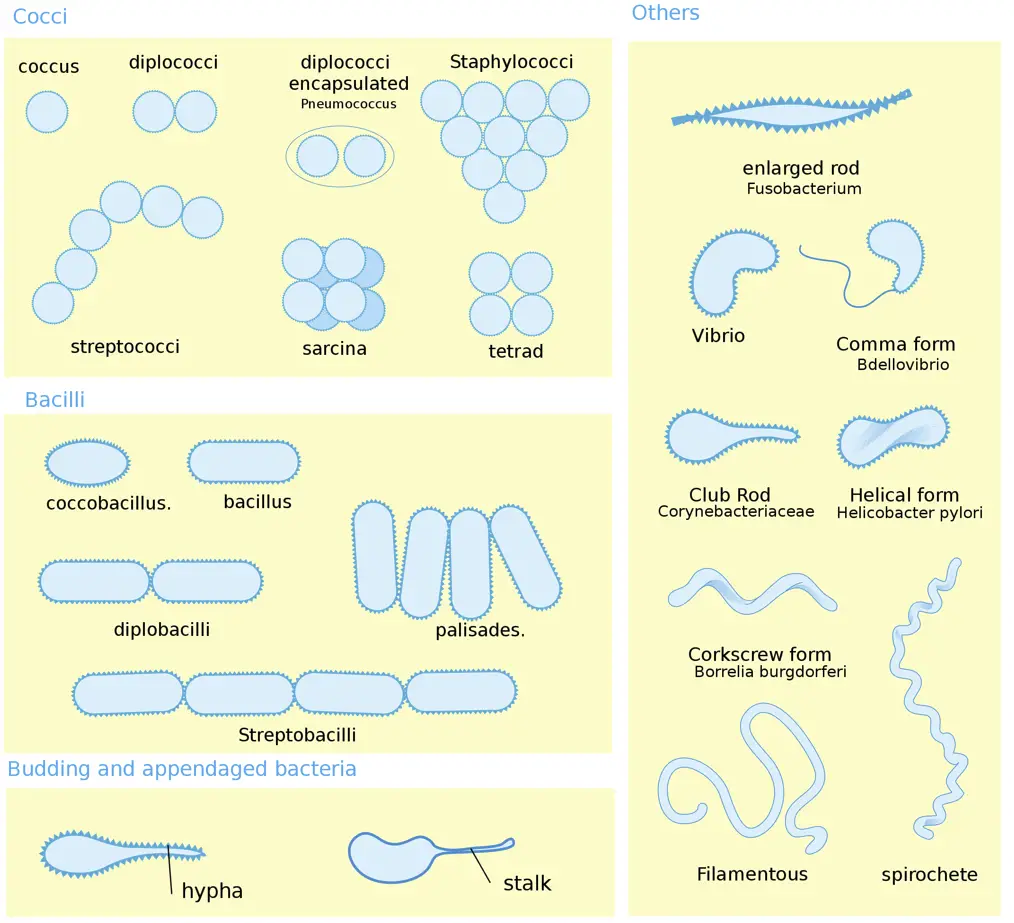
Klebsiella pneumoniae is a type of gram-negative bacteria that is commonly found in the human gut, where it is typically harmless. However, when it spreads to other parts of the body, such as the lungs, it can cause severe infections. This bacterium is encapsulated, which enhances its ability to resist the host’s immune response and contributes to its virulence. The presence of a thick polysaccharide capsule is a defining feature of the organism and key to its pathogenicity.
Habitat and Transmission
The primary habitat of Klebsiella pneumoniae is the gastrointestinal tract of humans. It can be transmitted in healthcare settings via person-to-person contact or through contaminated medical equipment. This pathogen is particularly notorious in hospitals, where it can spread through the hands of healthcare workers or by the use of invasive devices such as ventilators and urinary catheters.
Streptococcus Pneumoniae
General Characteristics
Streptococcus pneumoniae, also known as pneumococcus, is a gram-positive bacterium. This pathogen is most commonly associated with pneumonia, but it can also cause other types of infections such as meningitis and otitis media. Unlike Klebsiella, Streptococcus pneumoniae is part of the normal respiratory tract flora in many individuals, making it an opportunistic pathogen that can become problematic primarily in those with weakened immune systems.
Habitat and Transmission
Streptococcus pneumoniae is found in the upper respiratory tract of healthy individuals. It is spread primarily through airborne droplets when an infected person coughs or sneezes. Close contact with an infected individual can also facilitate the spread of this bacterium.
Infection Mechanisms
Klebsiella Infection
Entry and Spread
Klebsiella pneumoniae enters the body typically through the lungs or via medical devices. Once established, the bacteria can spread quickly, leading to severe localized infections or even systemic disease. Its capability to form biofilms on surfaces of medical devices further complicates treatment and eradication efforts.
Immune Response
The immune response to Klebsiella pneumoniae is often hampered by the bacterium’s robust defensive mechanisms, including its thick capsule which prevents phagocytosis. This results in a challenging situation for the immune system to clear the infection without significant intervention, such as antibiotics.
Streptococcus Infection
Entry and Spread
Streptococcus pneumoniae typically invades the body through the nasal or oral pathways. Following colonization, it can breach the epithelial barriers of the throat and enter the lungs or bloodstream, leading to more severe conditions.
Immune Response
The immune response to Streptococcus pneumoniae involves both the innate and adaptive arms of the immune system. The bacteria’s polysaccharide capsule is a key target for antibody-mediated immunity. Vaccination helps in the development of these antibodies, which play a crucial role in preventing infection by this pathogen.
Clinical Manifestations
Symptoms of Klebsiella
Common and Severe Symptoms
Infections caused by Klebsiella pneumoniae can range from mild to life-threatening. Common symptoms include fever, chills, and a productive cough with yellow or green sputum. Severe cases may result in breathlessness, rapid breathing, and even life-threatening complications like lung abscesses or septicemia.
Symptoms of Streptococcus
Common and Severe Symptoms
Streptococcus pneumoniae typically causes symptoms like cough, fever, shortness of breath, and chest pain. In more severe cases, symptoms can escalate to stiff neck, confusion, and a higher risk of complications such as meningitis or sepsis in individuals with weakened immune systems.
Diagnostic Approaches
Detecting Klebsiella
Laboratory Tests
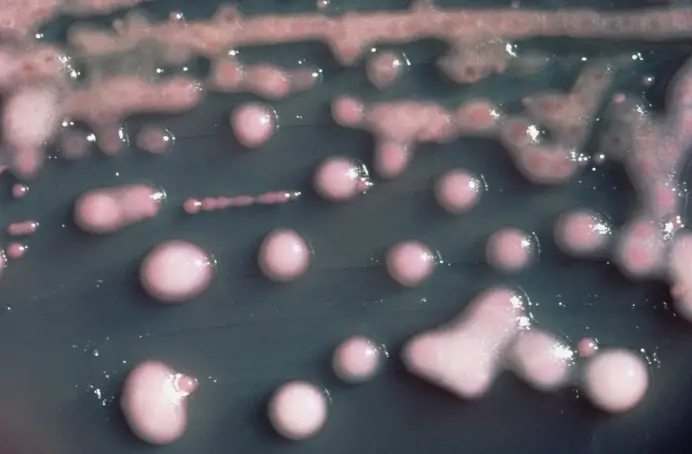
To identify Klebsiella pneumoniae, clinicians rely on culturing the bacteria from sputum or blood samples. Additional tests include antibiotic susceptibility testing to guide treatment due to the high resistance rates among strains.
Imaging Features
Chest X-rays or CT scans are used to assess lung involvement in suspected cases. These images can show elevated consolidation and abscess formation typical of Klebsiella infections.
Detecting Streptococcus
Laboratory Tests
Diagnosing Streptococcus pneumoniae involves bacterial cultures of respiratory fluids or blood. Polymerase chain reaction (PCR) tests may also be used for rapid detection.
Imaging Features
Imaging studies such as chest X-rays are instrumental in diagnosing pneumonia caused by Streptococcus pneumoniae. They typically reveal lobar consolidation, which helps distinguish this from other types of pneumonia.
Treatment Strategies
Treating Klebsiella Pneumoniae
Antibiotics and Resistance
Klebsiella pneumoniae is notoriously resistant to many standard antibiotics, making treatment challenging. The approach often involves the use of carbapenems, which are among the few antibiotics effective against strains resistant to more common drugs. However, the emergence of carbapenem-resistant Klebsiella (CRKP) has prompted the use of combination therapy:
- Polymyxins: These are often used as a last resort due to their nephrotoxic effects.
- Tigecycline: Effective in some cases but not recommended as a sole therapy for severe infections due to variability in efficacy.
- Aminoglycosides: Used in combination with other antibiotics to enhance bactericidal activity.
Testing for antibiotic susceptibility is crucial for determining the appropriate treatment regimen and managing resistance effectively.
Supportive Care
Supportive care is critical for patients suffering from Klebsiella pneumoniae infections, especially in severe cases:
- Respiratory support: Mechanical ventilation may be necessary for patients experiencing severe respiratory distress.
- Fluid management: Ensuring proper hydration and electrolyte balance helps support overall organ function and recovery.
- Nutritional support: High-calorie nutrition either orally or via feeding tubes can aid in recovery, especially for weakened patients.
Treating Streptococcus Pneumoniae
Antibiotics and Resistance
Treatment for Streptococcus pneumoniae typically involves penicillin or other beta-lactam antibiotics. However, resistance to these drugs has been increasing, leading to the use of alternative antibiotics such as:
- Macrolides: Effective but also facing rising resistance.
- Fluoroquinolones: Used for cases resistant to other antibiotics.
- Cephalosporins: Often used in severe cases, particularly for meningitis.
Early diagnosis and tailored antibiotic therapy are vital to manage the disease and prevent complications.
Supportive Care
Patients with Streptococcus pneumoniae infections often require:
- Oxygen therapy: To maintain adequate oxygen levels in the blood.
- Fluid replacement: To combat dehydration and maintain blood pressure.
- Pain management: Analgesics are administered to reduce discomfort from symptoms like chest pain and headaches.
Prevention Methods
Preventing Klebsiella Infection
Hygiene and Precautions
Preventing Klebsiella pneumoniae infections primarily involves stringent infection control practices, especially in healthcare settings:
- Hand hygiene: Regular and thorough hand washing or the use of alcohol-based hand sanitizers.
- Sterilization of medical equipment: Proper cleaning and sterilization to prevent contamination.
- Isolation protocols: Implementing strict isolation procedures for infected patients to prevent nosocomial spread.
Vaccination Status
Currently, there is no commercial vaccine available against Klebsiella pneumoniae, which emphasizes the importance of preventive measures and research towards vaccine development.
Preventing Streptococcus Infection
Hygiene and Precautions
Similar to preventing other respiratory infections, basic hygiene practices are effective:
- Cough etiquette: Covering mouth and nose during coughing or sneezing.
- Avoiding close contact: Staying away from people who are sick, especially in crowded places.
Vaccination Status
Vaccination is the most effective preventive measure against Streptococcus pneumoniae:
- Pneumococcal vaccines: Pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) are recommended, especially for children, older adults, and people with certain health conditions.
Public Health Impact
Epidemiology of Klebsiella
Klebsiella pneumoniae has become a significant public health concern due to its high drug resistance and association with hospital-acquired infections. It is prevalent in ICU settings and among patients with long-term care needs.
Epidemiology of Streptococcus
Streptococcus pneumoniae is a leading cause of bacterial pneumonia worldwide, especially in children under five and the elderly. It contributes significantly to morbidity and mortality globally, despite the availability of effective vaccines.
Healthcare Challenges
Both bacteria present considerable challenges in treatment and prevention, particularly in resource-limited settings. The rise of antibiotic resistance complicates the clinical management of infections and requires a coordinated global health response.
Future Directions
Research Trends
Ongoing research focuses on understanding the genetic mechanisms behind antibiotic resistance and developing new antimicrobial agents. Studies are also looking at the role of vaccines in reducing the incidence of infections caused by these bacteria.
Potential Breakthroughs
Future breakthroughs may include:
- Development of new vaccines: Especially against Klebsiella pneumoniae.
- Novel antibiotics: Targeting resistant strains more effectively.
- Rapid diagnostic tests: Enhancing the capability for quick and accurate detection to improve treatment outcomes.
FAQs
What causes Klebsiella pneumoniae?
Klebsiella pneumoniae infections are typically caused by bacteria found in the human intestines (where they do not cause disease) or in the environment. These infections often occur in healthcare settings, affecting patients with weakened immune systems or those with devices like ventilators.
How does Streptococcus pneumoniae spread?
Streptococcus pneumoniae spreads through respiratory droplets when an infected person coughs or sneezes. This bacterium can cause not only pneumonia but also ear and sinus infections, meningitis, and bloodstream infections, particularly in young children and the elderly.
What are the symptoms of Klebsiella pneumonia?
Symptoms of pneumonia caused by Klebsiella pneumoniae include severe cough, fever, chills, chest pain, and difficulty breathing. These infections can be particularly aggressive, leading to rapidly worsening conditions.
Can Streptococcus pneumoniae be prevented?
Yes, Streptococcus pneumoniae infections can be prevented with vaccines, which are particularly recommended for children, the elderly, and persons with certain chronic health conditions. Good hygiene practices, like regular hand washing, can also help reduce the spread.
Is Klebsiella pneumoniae antibiotic-resistant?
Klebsiella pneumoniae is known for its high level of resistance to multiple antibiotics, making it a challenging pathogen to treat. This resistance necessitates the need for careful antibiotic selection and may require combination therapy.
How serious is Streptococcus pneumoniae infection?
Infections caused by Streptococcus pneumoniae can range from mild to life-threatening. While healthy adults may experience mild symptoms, the elderly, infants, and those with weakened immune systems may develop severe complications like meningitis or bacteremia.
Conclusion
Recognizing and understanding the differences between Klebsiella pneumoniae and Streptococcus pneumoniae are paramount for effective clinical management and intervention. These pathogens, while both causing pneumonia, necessitate distinct approaches to treatment and prevention that can significantly impact patient outcomes.
Addressing these infections with targeted therapies, preventive vaccines, and informed healthcare practices can reduce the burden of disease and improve public health outcomes. The ongoing research and development in the field of infectious diseases remain crucial as these bacteria evolve and resistance patterns change.