In the medical field, precision and understanding of terminology can significantly impact patient care. Two terms often encountered in clinical settings are “infiltration” and “extravasation.” While they may sound similar, their implications and management are markedly different. Differentiating between these two phenomena is crucial for effective treatment and prevention of further complications.
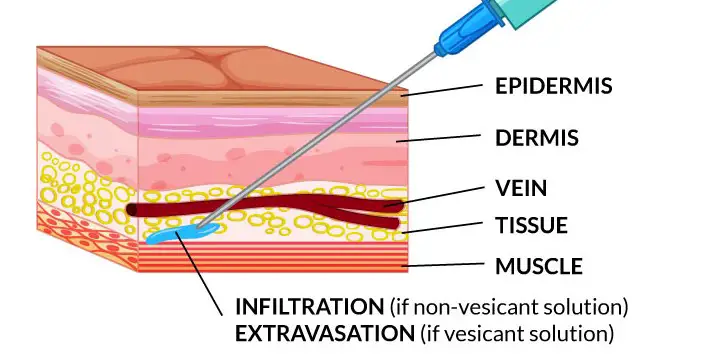
Infiltration occurs when fluid administered via an intravenous (IV) line leaks into the surrounding tissue. Extravasation, on the other hand, is a more severe form where the fluid leaking into the tissues is vesicant, causing damage and blistering. Recognizing the difference between these two is essential for prompt and appropriate medical response, potentially saving patients from serious harm.
The impact of these events extends beyond discomfort; they can lead to significant medical issues such as infections, delayed healing, and in severe cases, necrosis. Awareness and early detection are key in managing these complications, making knowledge of their distinct characteristics vital for healthcare professionals.
Definitions
What is Infiltration?
Infiltration in a medical context refers to an incident where fluid intended for intravenous (IV) delivery accidentally leaks into the surrounding tissues. This typically happens when the IV catheter becomes dislodged or is not properly inserted. The leaked fluid, usually saline, medication, or nutrients, builds up in the tissue leading to swelling and discomfort.
What is Extravasation?
Extravasation, unlike infiltration, involves the leakage of vesicant fluids. These fluids are capable of causing severe damage to tissues, including cellular death and tissue necrosis. Extravasation occurs under similar circumstances as infiltration but with more dire consequences due to the nature of the fluids involved.
Key Differences
In understanding the key differences between infiltration and extravasation, several aspects need consideration:
- Causes and Mechanisms: Infiltration is often a result of mechanical failure in the IV apparatus or improper placement. Extravasation, while it can also result from these issues, additionally involves the toxic nature of the fluid being administered.
- Types of Fluids Involved: Infiltration often involves non-vesicant fluids, which are generally less harmful, while extravasation involves vesicants which are highly damaging.
- Affected Areas: Both conditions affect the area around the IV site but the severity and type of tissue damage differ markedly.
Clinical Impact
The clinical impact of both conditions can vary greatly:
Complications of Infiltration
Complications from infiltration are typically less severe and include:
- Swelling and Discomfort: The most common symptoms where the area around the IV site becomes swollen and painful.
- Impaired Drug Delivery: The effectiveness of the drug can be reduced as it fails to enter the bloodstream properly.
Complications of Extravasation
Extravasation can lead to more severe complications, such as:
- Severe Pain and Blistering: The skin around the IV site may start to blister and become extremely painful.
- Tissue Necrosis: In severe cases, the affected tissues may die, which can require surgical intervention to remove the dead tissue.
Risk Factors
Patient-specific Risks
Some patients are more at risk of infiltration and extravasation due to:
- Vein Quality: Patients with fragile or small veins, like the elderly or neonates, are at higher risk.
- Health Conditions: Conditions such as diabetes or vascular diseases can increase risk due to compromised blood flow.
Procedure-related Risks
The likelihood of infiltration or extravasation can also increase due to:
- Skill of Healthcare Provider: Inexperienced practitioners may be more likely to incorrectly place IV lines.
- Duration and Frequency of IV Therapy: Long-term IV therapy or frequent IV changes increase the risk of complications.
Diagnosis Techniques
Initial Assessment Steps
The first step in diagnosing either infiltration or extravasation is a thorough assessment of the IV site. This includes:
- Visual Inspection: Checking for signs of swelling, redness, or leakage.
- Palpation: Feeling around the IV site for heat or excessive hardness, which may indicate underlying damage.
- Asking the Patient: Noting any complaints of pain or discomfort from the patient, which often precedes visible symptoms.
Diagnostic Tools Used
After initial assessment, several tools may be used to confirm and evaluate the severity of the condition:
- Ultrasound: This can help visualize fluid accumulation and tissue structure.
- Thermography: Detects heat patterns to identify inflamed areas.
- MRI or CT Scans: These are less commonly used but can provide detailed images of severe cases.
Management Strategies
Immediate Actions
Immediate management is critical to prevent further tissue damage:
- Stopping the Infusion: This is the first and most crucial step.
- Removing the IV Catheter: Careful removal to prevent additional injury.
- Elevating the Affected Limb: Reduces swelling and discomfort.
- Applying Cold or Warm Compresses: Depending on the type of fluid extravasated.
Long-term Care Options
For patients who experience severe infiltration or extravasation, long-term care might involve:
- Regular Monitoring: Frequent check-ups to assess healing and detect complications.
- Physical Therapy: Helps restore function and movement if mobility is affected.
- Surgical Intervention: In cases of severe tissue damage, surgery might be necessary to remove necrotic tissue or repair damage.
Prevention Tips
Best Practices in Clinical Settings
To prevent infiltration and extravasation, healthcare providers can adopt these best practices:
- Proper Catheter Selection and Placement: Use the correct type and size of catheter, placed by experienced personnel.
- Secure IV Lines Thoroughly: Ensure that the IV line is well secured to prevent accidental dislodgement.
- Regularly Rotate IV Sites: To minimize the risk of complications from prolonged IV placement.
Training and Education for Healthcare Professionals
Continuous training and education are crucial:
- Regular Workshops and Simulations: Keeps skills sharp and up to date.
- Learning from Past Incidents: Reviewing case studies within the healthcare facility to learn from previous mistakes.
Case Studies
Examples of Infiltration
- Case Study 1: A patient receiving hydration therapy experienced swelling and pain due to an improperly secured IV line, diagnosed early and managed with minimal intervention.
- Case Study 2: A neonatal patient showed signs of infiltration due to fragile veins. Prompt detection and response led to a quick resolution without long-term effects.
Examples of Extravasation
- Case Study 3: An oncology patient receiving chemotherapy suffered extravasation, leading to severe local tissue damage. Immediate cessation of the infusion and application of antidotes minimized tissue loss.
- Case Study 4: A patient in the emergency department experienced extravasation from an antibiotic, which was treated by cold compresses and elevation, preventing severe complications.
Frequently Asked Questions
What is Infiltration?
Infiltration refers to the unintentional administration of non-vesicant solutions into surrounding tissue due to an IV catheter becoming dislodged or misplaced. This typically results in swelling, discomfort, and slowed infusion rates but is generally less harmful than extravasation.
What is Extravasation?
Extravasation is the accidental infusion of vesicant drugs into the tissue surrounding the IV site. These drugs can cause severe local tissue damage, including pain, blisters, and even tissue death, necessitating immediate and aggressive treatment.
How do you treat Extravasation?
The treatment of extravasation begins with immediate cessation of the infusion followed by careful removal of the catheter. The affected area should be treated with specific antidotes or therapies depending on the extravasated medication, and it may require surgical intervention in severe cases.
How can Infiltration be prevented?
Preventing infiltration involves regular monitoring of IV sites for signs of inflammation or leakage, proper catheter placement and securement, and training healthcare providers to recognize early signs of complications.
What are the long-term effects of Extravasation?
The long-term effects of extravasation can include severe tissue damage leading to scarring, loss of function, and in extreme cases, amputation. Early detection and treatment are crucial to minimize these severe outcomes.
Conclusion
Differentiating between infiltration and extravasation in clinical practice is not just about terminology but about ensuring patient safety and quality of care. Recognizing the subtle differences between these two conditions can significantly affect outcomes, highlighting the need for vigilance and education among healthcare professionals.
This article underscores the importance of accurate diagnosis and effective management strategies in dealing with infiltration and extravasation. As medical professionals, continuous education and adherence to best practices are indispensable in preventing these potentially harmful occurrences in patient care settings.
