Skin conditions, though often overlooked, can significantly affect an individual’s quality of life. Among the myriad of dermatological terms and diagnoses, Hyperkeratosis and Parakeratosis stand out due to their prevalence and impact on skin health. These terms describe different types of skin abnormalities, primarily affecting the epidermis, the outermost layer of the skin.
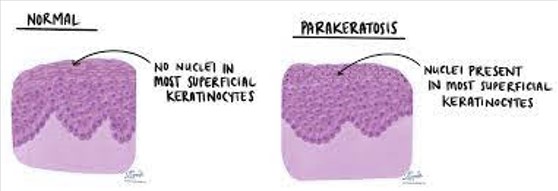
Hyperkeratosis is characterized by the thickening of the stratum corneum, the outermost layer of the epidermis, due to an excess production of keratin. Parakeratosis, on the other hand, refers to a condition where there is an abnormal maturation of the skin cells, leading to the presence of nuclei in the stratum corneum. While both conditions involve the epidermis, their causes, symptoms, and treatments vary.
The health of our skin is a reflection of numerous factors, including genetics, environment, and lifestyle choices. Hyperkeratosis and Parakeratosis are examples of how our skin can react to these factors. Although they share some similarities, understanding the distinctions between them is crucial for effective treatment and management. This article aims to shed light on these differences, helping individuals navigate their skin health with more knowledge and confidence.

Skin Anatomy 101
The Epidermis Layer
The epidermis is the outermost layer of the skin, serving as the body’s first line of defense against environmental threats. It’s composed of keratinocytes, cells that produce keratin, a protein that gives skin its strength and resilience. The epidermis is responsible for the skin’s waterproofing and plays a key role in skin pigmentation, hosting the melanocytes that produce melanin.
Structure and Function
The epidermis itself is divided into several sub-layers, from the deep basal layer where cells are born, to the stratum corneum at the surface, made up of dead keratinocytes. This top layer acts as a barrier to protect the underlying tissues from infection, dehydration, and physical damage.
Keratinization Process
Keratinization is the process by which keratinocytes mature and move up through the layers of the epidermis, eventually dying and forming a protective layer. This cycle is critical for skin health, as it helps to repair wounds, renew the skin surface, and maintain the barrier against the outside world.
Normal Skin Renewal Process
On average, the skin renewal cycle takes about 28 days. New cells form in the basal layer and take roughly four weeks to migrate to the surface, where they flake off. This constant renewal helps to keep the skin smooth, clear, and capable of performing its protective functions.
What is Hyperkeratosis?
Definition
Hyperkeratosis is a condition characterized by the thickening of the skin’s outer layer due to an excess of keratin. This can result in rough, dry, or thickened patches of skin, often in response to friction, pressure, or other irritants.
Basic Understanding
This condition reflects an abnormality in the keratinization process, where the balance of skin cell production and shedding is disrupted. Hyperkeratosis can occur as a localized patch or more widely across the body, depending on its cause.
Causes
Factors contributing to hyperkeratosis include genetic predispositions, chronic skin irritation, exposure to harmful substances, and prolonged pressure on the skin. In some cases, it may also be linked to underlying health conditions or nutritional deficiencies.
Symptoms
Symptoms of hyperkeratosis encompass thickened skin, calluses, corns, and areas of rough texture. These patches may be painless or sensitive and vary greatly in their appearance and severity.
Types of Hyperkeratosis
- Calluses and corns typically form on the hands and feet due to repeated friction.
- Actinic keratosis arises after prolonged sun exposure, a precancerous condition that can lead to skin cancer if left untreated.
What is Parakeratosis?
Definition
Parakeratosis is a condition where the keratinization process is incomplete, resulting in the retention of nuclei in the cells of the stratum corneum. Unlike hyperkeratosis, parakeratosis often indicates an underlying pathological process.
Basic Understanding
This condition signifies an abnormality in skin cell differentiation and shedding. It’s frequently associated with inflammatory skin diseases and is often observed in skin biopsies as a diagnostic clue.
Causes
Causes of parakeratosis include skin inflammation, vitamin A deficiency, and chronic exposure to irritants. It is also common in certain skin conditions like psoriasis.
Symptoms
Parakeratosis manifests as scaly, red patches that may itch or hurt. These areas are indicative of a disruption in the normal skin barrier, leading to potential sensitivity or susceptibility to infection.
Types of Parakeratosis
- Psoriasis involves rapid skin cell turnover, leading to thick, scaly patches.
- Parakeratosis pustulosa is characterized by scaly patches that may also feature pustules.
Key Differences
Cellular Level
At the cellular level, Hyperkeratosis and Parakeratosis differ in how skin cells proliferate and mature. Hyperkeratosis is characterized by an overproduction of keratin, leading to a thickened stratum corneum. In contrast, Parakeratosis involves the retention of nuclei in the stratum corneum cells, indicating incomplete keratinization. These changes not only affect the skin’s appearance but also its function and response to treatment.
Clinical Presentation
The visual and symptomatic differences between these conditions are stark. Hyperkeratosis typically presents as thick, rough patches of skin, while Parakeratosis areas are red, scaly, and sometimes itchy. Recognizing these signs is crucial for early diagnosis and management.
Causes and Triggers
Environmental and genetic factors play roles in both conditions but in differing capacities. Hyperkeratosis may be more closely linked to external pressures and friction, whereas Parakeratosis often results from internal disease processes or nutritional deficiencies.
Treatment Approaches
Medical Interventions and Home Care
For Hyperkeratosis, topical treatments and lifestyle modifications can reduce symptoms. Parakeratosis treatment, however, might require more aggressive medications or UV therapy to address the underlying inflammation or deficiency.
Diagnosis and Management
Diagnostic Techniques
Early diagnosis involves a combination of biopsy and visual inspection. A biopsy can reveal the characteristic cellular changes of each condition, aiding in accurate diagnosis and tailored treatment plans.
Treatment Options for Hyperkeratosis
Treatment may include:
- Moisturizers and keratolytic agents to soften the skin
- Physical therapies like cryotherapy for lesions
- Lifestyle changes to reduce friction and pressure
Treatment Options for Parakeratosis
Parakeratosis treatments focus on addressing the root cause:
- Topical steroids to reduce inflammation
- Vitamin supplements if deficiency is a factor
- Phototherapy for severe cases
Preventive Measures
Maintaining skin health is key in preventing both conditions:
- Regular moisturizing
- Sun protection to prevent actinic keratosis
- Avoidance of excessive friction and pressure
Case Studies
Hyperkeratosis Case Example
A patient presented with thick, hardened skin on the heel due to prolonged standing. Treatment involved custom orthotics, regular exfoliation, and moisturizing, resulting in significant improvement.
Parakeratosis Case Example
A case of psoriasis-induced Parakeratosis was managed with topical corticosteroids and vitamin D analogs, along with UVB phototherapy, showing considerable lesion reduction and symptom relief.
Frequently Asked Questions
What causes Hyperkeratosis?
Hyperkeratosis is typically caused by chronic friction, pressure, or irritation to the skin. It can also result from genetic conditions, sun damage, and certain skin diseases. Lifestyle factors, such as poor hygiene or the use of harsh skincare products, can further exacerbate the condition.
How is Parakeratosis diagnosed?
Parakeratosis is diagnosed through a clinical examination and confirmed with a biopsy. A dermatologist will examine the affected skin and may take a small sample to observe the characteristic retention of nuclei in the stratum corneum under a microscope, which confirms the diagnosis of Parakeratosis.
Can Hyperkeratosis and Parakeratosis be cured?
While there is no definitive cure for Hyperkeratosis or Parakeratosis, many treatments are available to manage symptoms and minimize the effects. Treatment options range from topical creams and ointments to more advanced procedures like laser therapy, depending on the severity and underlying cause of the condition.
Are Hyperkeratosis and Parakeratosis contagious?
No, neither Hyperkeratosis nor Parakeratosis is contagious. These conditions are related to the abnormal production or maturation of skin cells and are not caused by pathogens that can be transmitted from person to person.
Conclusion
Understanding the differences between Hyperkeratosis and Parakeratosis is pivotal for anyone looking to maintain or improve their skin health. Both conditions, while not life-threatening, can cause discomfort and affect an individual’s self-esteem. Awareness and proper management are key to living with these conditions.
By seeking professional advice and adhering to a treatment plan, individuals can significantly reduce the symptoms associated with Hyperkeratosis and Parakeratosis. Remember, skin health is a vital part of overall well-being, and taking proactive steps towards understanding and treating skin conditions is always beneficial.

