Neural tube defects (NTDs) are severe birth defects affecting the brain and spinal cord, among which exencephaly and anencephaly stand out due to their critical impact on fetal development. These conditions, while distinct, share a common origin during the early stages of embryonic growth, leading to varying degrees of brain development issues and skull formation.
Exencephaly and anencephaly are two different manifestations of neural tube defects. Exencephaly occurs when the brain is exposed outside the skull due to incomplete closure of the neural tube, potentially transitioning into anencephaly as pregnancy progresses, where most of the brain and skull do not develop. Anencephaly, one of the most severe neural tube defects, results in a baby born without major portions of the brain, skull, and scalp.
The differences between these conditions, though medically significant, revolve around the developmental stage of the neural tube defect, the presence and formation of brain tissue, and the structural integrity of the skull. Understanding these distinctions is vital for diagnosis, management, and exploring avenues for prevention and research into neural tube defects.
Exencephaly Explained
Definition and Basics
Exencephaly is a neural tube defect (NTD), a type of congenital anomaly where the brain is exposed to the amniotic fluid due to a failure in the skull to close completely. This condition occurs during the early stages of fetal development, specifically within the first few weeks of pregnancy. Exencephaly is often considered a precursor to anencephaly, another severe neural tube defect, as the exposed brain tissue can degenerate over time, leading to anencephaly.
How Exencephaly Develops
Exencephaly develops due to the neural tube failing to close at the top. The neural tube is the precursor to the central nervous system, comprising the brain and spinal cord. The closure process should complete by the 28th day post-conception, but in cases of exencephaly, this closure is incomplete at the cranial end. The development of exencephaly is influenced by a combination of genetic, environmental factors, and nutritional deficiencies in the mother, notably a lack of folic acid.
- Steps in the development of exencephaly:
- The neural plate fails to form the neural tube properly.
- The cranial end of the neural tube remains open.
- Brain tissue develops and grows outside the skull.
Symptoms and Diagnosis
Symptoms of exencephaly are visually apparent, with the brain tissue being exposed outside of the skull without any covering of skin or bone. Due to the exposure to the amniotic fluid, the brain tissue is susceptible to damage, leading to further complications or transition into anencephaly.
Diagnosis of exencephaly is primarily done through prenatal ultrasound imaging, which can detect the condition as early as the first trimester. Further diagnostic tests, such as amniocentesis, may be conducted to assess any additional genetic abnormalities.
Anencephaly Uncovered
Definition and Essentials
Anencephaly is a severe, lethal condition characterized by the absence of a major portion of the brain, skull, and scalp. This defect occurs during fetal development and is apparent at birth. Anencephaly results when the neural tube, which forms the early brain and spinal cord, fails to close completely at one end. The upper part, where the brain and skull would normally develop, does not form correctly, if at all.
Formation and Causes
The formation of anencephaly, similar to exencephaly, is attributed to the incomplete closure of the neural tube during the first month of pregnancy. The exact causes of this failure are not fully understood but are believed to be a mix of genetic predispositions and environmental factors, such as:
- Lack of folic acid in the mother’s diet before and during early pregnancy
- Genetic mutations affecting neural tube development
- Environmental toxins the mother may be exposed to during pregnancy
Symptoms and Identification
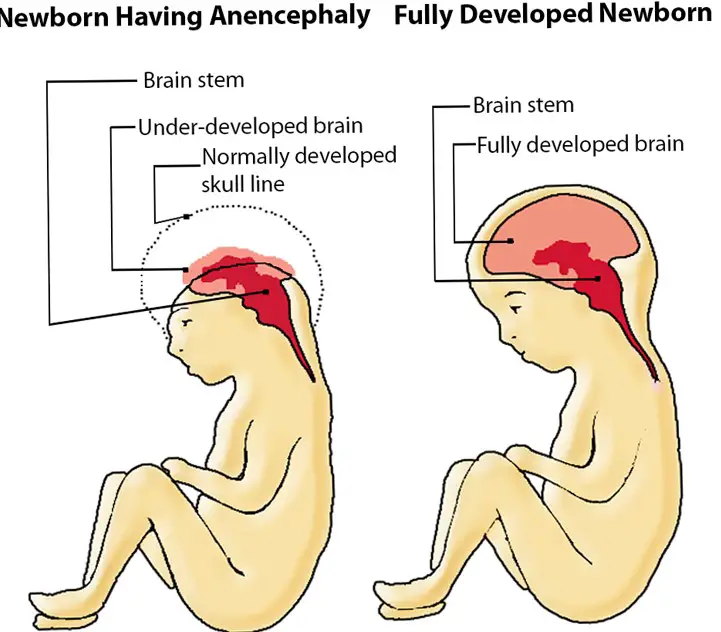
The primary symptom of anencephaly is a significant absence of the brain and skull. In some cases, the baby may have rudimentary brainstem function, but the upper parts of the brain (cerebral hemispheres and cerebellum) are missing. This condition is easily identifiable at birth due to these physical abnormalities.
Identification of anencephaly before birth can be achieved through prenatal screening tests, such as ultrasound. Advanced imaging techniques and genetic testing offer further insights into the condition’s specifics and any additional complications.
Key Differences
Structural Distinctions
The structural distinctions between exencephaly and anencephaly lie in the presence and condition of the brain tissue. In exencephaly, the brain is present but exposed outside the skull due to incomplete skull formation. In contrast, anencephaly involves a substantial or complete lack of the brain and skull above the base, with no protective covering or significant brain tissue present.
Developmental Timelines
The developmental timeline is a critical differentiator. Exencephaly occurs first and may progress to anencephaly as the pregnancy advances. The transition from exencephaly to anencephaly involves the degeneration of exposed brain tissue, leading to the more severe condition of anencephaly.
Diagnostic Criteria
While both conditions are detectable through prenatal ultrasound, the diagnostic criteria differ based on the visible structural abnormalities. For exencephaly, the diagnosis centers around the observation of brain tissue outside the skull. For anencephaly, the diagnosis is made based on the absence or severe reduction of the brain and skull.
Risk Factors
Genetic Considerations
Genetic factors play a significant role in the development of neural tube defects like exencephaly and anencephaly. While not all cases can be directly linked to hereditary patterns, families with a history of NTDs may have an increased risk. Mutations in genes related to folic acid metabolism are particularly important, highlighting the role of genetics in these conditions.
Environmental Triggers
Environmental factors are also crucial in understanding the risk associated with neural tube defects. Exposure to certain chemicals, medications, and toxins during pregnancy can significantly increase the risk. Additionally, high temperatures in the form of fevers or use of hot tubs and saunas by pregnant women have been associated with a higher incidence of these conditions.
Maternal Health Influences
The health and nutritional status of the mother before and during pregnancy significantly affect the risk of exencephaly and anencephaly. Obesity, diabetes, and poor nutrition—especially inadequate intake of folic acid—are known risk factors. Furthermore, untreated chronic conditions and certain medications can contribute to the development of these birth defects.
Impact and Prognosis
Life Expectancy and Quality
Babies born with anencephaly have a very limited life expectancy, often measured in hours or days after birth, due to the lack of vital brain structures. In contrast, exencephaly is typically fatal during gestation or transitions into anencephaly before birth. These conditions profoundly affect families, emotionally and psychologically.
Treatment Options
Treatment for these conditions is primarily palliative, focusing on the comfort of the baby and support for the family. There are no curative treatments available for anencephaly or exencephaly, given their fatal prognosis. In some cases, management of pregnancy may involve discussions on the continuation of the pregnancy and palliative care options post-birth.
Support and Care
Support for families affected by these diagnoses is crucial. This can include counseling, bereavement support, and care planning. Connecting with support groups and organizations dedicated to neural tube defects can provide emotional support and resources for navigating this challenging journey.
Prevention Strategies
Prenatal Care and Tests
Regular prenatal care is essential for early detection and management of neural tube defects. This includes routine ultrasounds and blood tests that can identify markers indicative of these conditions. Early diagnosis provides families with information and time to make informed decisions regarding care and support.
Nutritional Guidelines
Nutrition plays a key role in preventing neural tube defects. The most effective prevention strategy is the consumption of folic acid before conception and during early pregnancy. Women of childbearing age are advised to take daily supplements of folic acid in addition to eating folic-acid-rich foods to reduce the risk of NTDs.
- Folic Acid Recommendations:
- 400 micrograms (mcg) daily before conception
- 600 mcg daily during pregnancy
Research and Advances
Ongoing research into neural tube defects aims to uncover the complex interplay of genetic, environmental, and nutritional factors involved. Advances in genetic screening and prenatal diagnostics are improving early detection rates. Studies into new treatment and prevention methods, including the potential for in utero surgery and enhanced nutritional supplementation, hold promise for reducing the incidence of these conditions in the future.
Frequently Asked Questions
What causes exencephaly and anencephaly?
Exencephaly and anencephaly are caused by the neural tube’s failure to close completely during early fetal development. Factors contributing to this include genetic mutations, environmental influences, and maternal nutritional deficiencies, especially in folic acid.
Can exencephaly or anencephaly be detected before birth?
Yes, both exencephaly and anencephaly can often be detected before birth through routine prenatal screenings and diagnostic tests such as ultrasound and maternal blood tests. Early detection is crucial for managing the pregnancy and preparing for the outcomes.
Are there any treatments for exencephaly or anencephaly?
While there is no cure for anencephaly and treatment options for exencephaly are extremely limited, care is focused on providing comfort and support. For anencephaly, the focus is on palliative care due to the condition’s fatal prognosis shortly after birth.
How can the risk of neural tube defects be reduced?
The risk of neural tube defects like exencephaly and anencephaly can be significantly reduced by taking folic acid supplements before conception and during early pregnancy. Adequate intake of folic acid has been shown to greatly decrease the risk of NTDs.
Conclusion
The distinctions between exencephaly and anencephaly highlight the complexity of neural tube defects and the importance of early diagnosis and management. These conditions underscore the critical need for ongoing research, awareness, and preventive measures to mitigate the risk of such devastating outcomes.
By fostering a better understanding of these conditions and their implications, we can improve the support for affected families and enhance the prospects for prevention. Continued advancements in prenatal care, coupled with increased awareness about the significance of nutritional supplementation, hold the promise of reducing the incidence of these and other neural tube defects, offering hope for future generations.

