The human body is a complex system, with each component playing a crucial role in maintaining health. Among these components, the pancreas is a vital organ that regulates blood sugar levels through its unique cells. The focus of our exploration will be the alpha and beta cells, two types of cells within the pancreas that have critical but distinct functions in the process of glucose regulation.
Alpha and beta cells are specialized cells located in the pancreas, primarily responsible for maintaining glucose homeostasis in the body. Alpha cells produce the hormone glucagon, which raises blood glucose levels, while beta cells produce insulin, which lowers blood glucose levels. Their coordinated actions ensure that the body’s energy needs are met while preventing the harmful effects of too high or too low blood sugar.
These cells’ significance extends beyond their roles in glucose regulation; they are also central to understanding diseases such as diabetes. The dysfunction or destruction of beta cells leads to Type 1 diabetes, whereas impaired insulin action and eventual beta cell failure contribute to Type 2 diabetes. Exploring the differences between alpha and beta cells sheds light on their essential functions and their impact on overall health.
Pancreas Overview
Pancreas Role
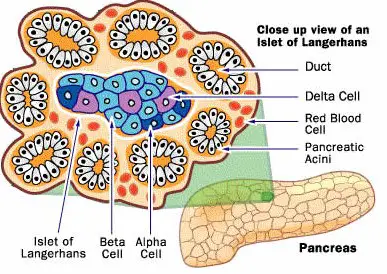
The pancreas is a vital organ nestled in the abdomen, playing a crucial role in digestion and glucose regulation. It functions as both an exocrine and an endocrine gland. The exocrine part secretes digestive enzymes that aid in breaking down food in the small intestine. Meanwhile, the endocrine part, comprising small clusters of cells known as islets of Langerhans, is responsible for maintaining blood sugar levels through the production of key hormones.
Cells Composition
Within the islets of Langerhans, there are several types of cells, each with a unique role in the body’s metabolic processes. The most prominent are alpha cells and beta cells. Alpha cells produce the hormone glucagon, which raises blood glucose levels, while beta cells produce insulin, crucial for lowering blood glucose. Other cell types, such as delta cells (secreting somatostatin) and PP cells (producing pancreatic polypeptide), also play roles in regulating various bodily functions.
Alpha Cells
Location and Structure
Alpha cells are found predominantly in the outer rim of the islets of Langerhans. These cells are characterized by their granular appearance under a microscope, due to the presence of secretory granules containing glucagon.
Hormone Production: Glucagon
Glucagon’s primary function is to increase blood glucose levels by promoting the breakdown of glycogen to glucose in the liver. This process is known as glycogenolysis. Glucagon also aids in the formation of glucose from amino acids and other substrates, a process called gluconeogenesis.
Function and Regulation
The release of glucagon by alpha cells is principally regulated by blood glucose levels. When blood glucose is low, alpha cells secrete glucagon, which then acts on the liver to increase blood glucose. This mechanism ensures a constant supply of glucose for the body, especially for the brain, which relies almost exclusively on glucose for energy.
Beta Cells
Location and Structure
Beta cells constitute the majority of the cells in the islets of Langerhans and are found more centrally within these islets. Similar to alpha cells, they contain granules; however, these granules store insulin.
Hormone Production: Insulin
Insulin is the key hormone responsible for lowering blood glucose levels. It facilitates the uptake of glucose by cells, especially muscle and fat cells, and inhibits the liver’s production of glucose.
Function and Regulation
The release of insulin by beta cells is tightly regulated by blood glucose levels. High glucose levels stimulate beta cells to release insulin, which then helps cells absorb glucose, lowering the glucose in the bloodstream. This process is critical for maintaining the body’s energy balance and ensuring that cells receive the glucose they need to function.
Key Differences
Hormonal Differences
The most striking difference between alpha and beta cells lies in the hormones they produce: glucagon and insulin, respectively. These hormones have opposite effects on blood glucose levels, with glucagon increasing and insulin decreasing it.
Physiological Roles
Alpha cells play a key role in preventing hypoglycemia by ensuring that glucose levels do not fall too low. Conversely, beta cells prevent hyperglycemia by reducing high blood glucose levels to a normal range.
Response to Glucose
Alpha and beta cells have contrasting responses to glucose. Alpha cells are activated to secrete glucagon when glucose levels are low, whereas beta cells respond to high glucose levels by releasing insulin. This dynamic balance is crucial for maintaining homeostasis and ensuring the body’s proper metabolic functioning.
Interaction and Balance
Coordinated Regulation
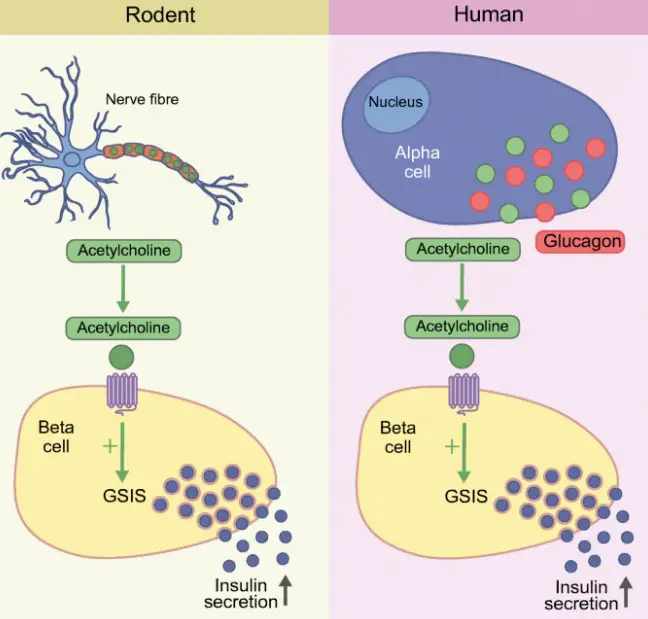
The body’s ability to maintain balanced blood sugar levels hinges on the synchronized actions of alpha and beta cells. This coordination ensures that glucose levels remain within a healthy range, preventing both high and low blood sugar. The interaction involves several hormones and signals beyond insulin and glucagon, including somatostatin from delta cells, which can inhibit both insulin and glucagon release, adding another layer of regulation.
Impact on Blood Sugar Levels
The balance between insulin and glucagon is critical for blood sugar management. Insulin helps to lower blood sugar after meals by facilitating glucose uptake by cells, while glucagon raises blood sugar during fasting periods by signaling the liver to release stored glucose. This balance ensures that the body’s cells have a steady supply of energy and that blood sugar levels remain stable.
Health Implications
Diabetes
Type 1: Beta Cell Destruction
Type 1 diabetes is characterized by the autoimmune destruction of beta cells, leading to insufficient insulin production. This results in high blood sugar levels, as glucose cannot be effectively taken up by the cells. Managing type 1 diabetes requires lifelong insulin therapy to replace the hormone that the body can no longer produce.
Type 2: Insulin Resistance and Beta Cell Failure
In type 2 diabetes, the body’s cells become resistant to insulin, and over time, beta cells fail to produce enough insulin to overcome this resistance. This form of diabetes is often associated with obesity, poor diet, and lack of exercise. Treatment focuses on diet, exercise, and medications that improve insulin sensitivity or insulin secretion.
Other Conditions
Hypoglycemia: Alpha Cell Dysfunction
Hypoglycemia, or low blood sugar, can occur if alpha cells do not properly secrete glucagon in response to low glucose levels. Without glucagon’s action to raise blood sugar, individuals may experience symptoms such as shaking, sweating, and in severe cases, loss of consciousness.
Pancreatic Disorders
Various pancreatic disorders, including pancreatitis and pancreatic cancer, can impact the functioning of alpha and beta cells, disrupting the delicate balance of glucose regulation and leading to metabolic issues.
Research and Innovation
Recent Studies
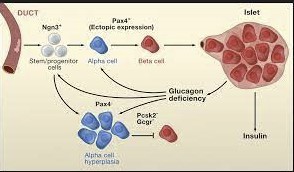
Recent advancements in the field have focused on understanding the cellular mechanisms behind diabetes, exploring new treatments that can either protect beta cells, improve their function, or replace them entirely. Studies on alpha cells have also gained traction, especially concerning their role in hypoglycemia prevention.
Future Directions
Future research aims to develop regenerative therapies that could restore normal cell function in diabetic patients, potentially offering a cure for types 1 and 2 diabetes. Innovations in islet cell transplantation, stem cell therapy, and artificial pancreas technology hold promise for revolutionizing diabetes management.
Managing Health
Diet and Lifestyle
A balanced diet and active lifestyle are key to maintaining healthy blood sugar levels. Recommendations include:
- Consuming a diet rich in fiber, whole grains, and lean proteins.
- Limiting intake of sugary and processed foods.
- Regular physical activity to improve insulin sensitivity.
Medical Interventions
For those with diabetes or at risk, medical interventions might include:
- Medications that increase insulin sensitivity or stimulate insulin production.
- Insulin therapy for individuals who cannot produce enough insulin.
- Monitoring blood sugar levels regularly to manage and adjust treatment plans accordingly.
Frequently Asked Questions
What are Alpha Cells?
Alpha cells are pancreatic cells that produce glucagon, a hormone that increases blood glucose levels by promoting the breakdown of glycogen to glucose in the liver. These cells play a vital role in preventing hypoglycemia by ensuring that glucose is released into the bloodstream when needed.
How do Beta Cells Function?
Beta cells are located in the pancreas and are responsible for producing insulin, a hormone crucial for lowering blood glucose levels. Insulin facilitates the uptake of glucose by cells, thus reducing blood sugar and providing energy to the body’s cells. The proper functioning of beta cells is essential for maintaining glucose homeostasis.
Can Alpha and Beta Cells Regenerate?
Regeneration of alpha and beta cells is an area of ongoing research. While the adult pancreas has a limited capacity to regenerate these cells, certain conditions and treatments can promote their regeneration. This potential for regeneration offers hope for new treatments for diabetes and other pancreatic disorders.
What Causes Alpha and Beta Cell Dysfunction?
Dysfunction in alpha and beta cells can result from genetic factors, autoimmune responses, or environmental triggers such as obesity and chronic stress. These disruptions can lead to the overproduction or insufficient production of glucagon and insulin, respectively, affecting blood glucose levels and potentially leading to diabetes.
Conclusion
Understanding the difference between alpha and beta cells is fundamental to comprehending how the body regulates blood sugar and what goes awry in diabetes. These cells’ coordinated efforts are essential for maintaining energy balance and ensuring our body functions optimally. By exploring the roles and mechanisms of alpha and beta cells, we gain insights into preventive measures and treatments for diabetes, enhancing our ability to manage this condition effectively.
The implications of alpha and beta cell functions extend beyond individual health, touching on broader medical and research fields. Innovations in treating diabetes and other metabolic disorders are increasingly focusing on how to protect, enhance, or replace the functions of these cells. Our journey through the complexities of alpha and beta cells not only enriches our understanding of the human body but also highlights the potential for groundbreaking advancements in health and medicine.