White blood cells (WBCs) and platelets play crucial roles in the body’s defense and healing mechanisms. While white blood cells are the soldiers of the immune system, fighting off infections and invaders, platelets are the medics, responsible for blood clotting and wound repair. These two components of the blood, though functionally distinct, share a complex relationship that influences both health and disease states.
The relation between WBCs and platelets is not just a matter of numerical balance but involves a dynamic interaction that affects the body’s response to injury and infection. An increase or decrease in the count of one can significantly impact the function and effectiveness of the other. For instance, certain infections can lead to an increase in white blood cells, which, in turn, might affect platelet function or production.
At the heart of their relationship is the bone marrow, where both WBCs and platelets are produced. Disorders that affect bone marrow function can lead to abnormalities in the production and balance of these cells, impacting the body’s ability to fight infections and clot blood. This intricate interplay is crucial for maintaining homeostasis and ensuring that the body can respond effectively to challenges such as injury, inflammation, and infection.
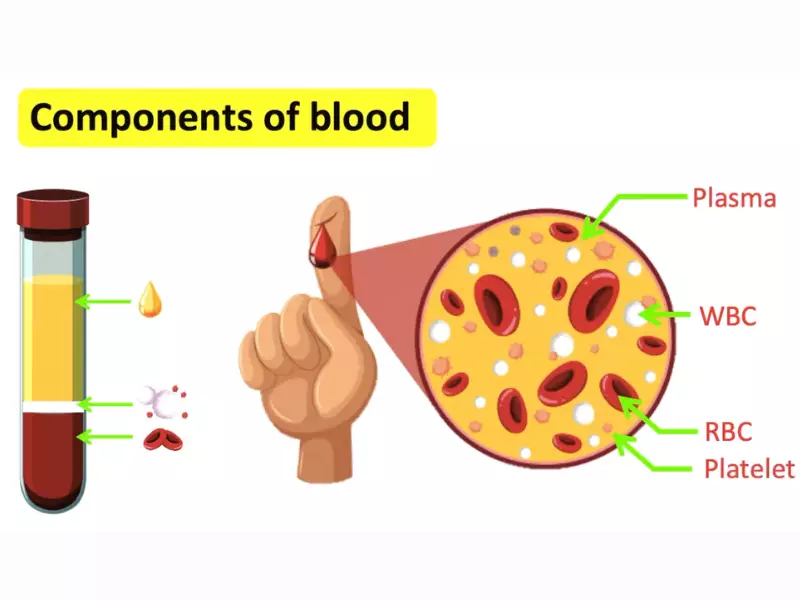
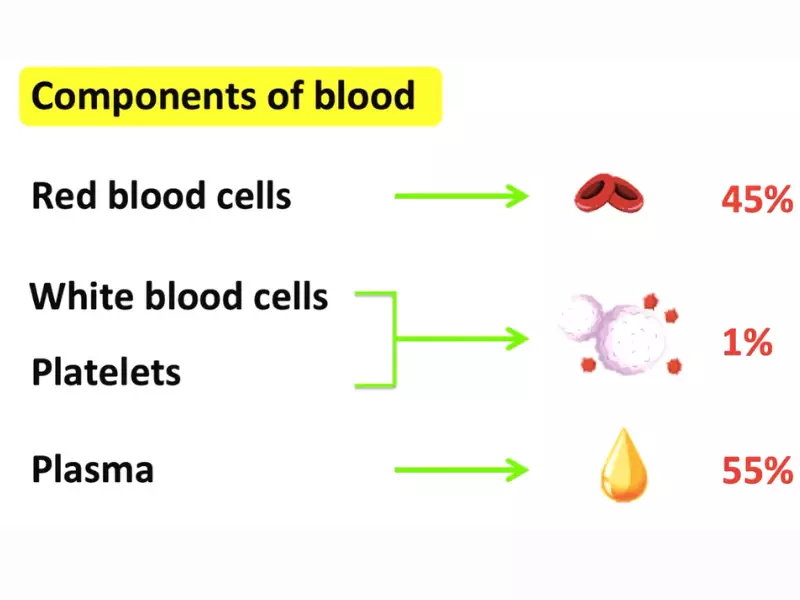
Blood Basics
Blood, a vital liquid flowing through our veins, plays a crucial role in our body’s overall functioning. It’s composed of various components, each with a unique and essential role in maintaining health and combating diseases.
Blood Components
Red Blood Cells (RBCs)
RBCs, or erythrocytes, are responsible for carrying oxygen from the lungs to the body’s tissues and returning carbon dioxide back to the lungs for exhalation. Their high count reflects the body’s efficiency in oxygen transport.
White Blood Cells (WBCs)
WBCs, or leukocytes, are the body’s defense force against infections and foreign invaders. They vary in type and function, each designed to combat different pathogens or health conditions.
Platelets
Platelets, or thrombocytes, are tiny blood cells crucial for blood clotting. They work to prevent excessive bleeding when we are injured.
Plasma
Plasma is the liquid component of blood, comprising water, salts, and proteins. It serves as a transport medium for blood cells, nutrients, hormones, and waste products.
Function of WBCs
Immune Response
WBCs play a pivotal role in the immune system, identifying and neutralizing pathogens like bacteria, viruses, and fungi.
Types of WBCs
There are several types of WBCs, including neutrophils, lymphocytes, monocytes, eosinophils, and basophils, each serving a specific role in the immune response and inflammation process.
Function of Platelets
Blood Clotting
Platelets initiate the clotting process by aggregating at a wound site, forming a plug to stop bleeding. This is crucial for wound healing and preventing blood loss.
Platelet Count Significance
The platelet count is an important diagnostic tool, as too few or too many platelets can indicate a range of health issues, from bleeding disorders to thrombotic risks.
WBC and Platelet Interaction
Role in Hemostasis
WBCs and platelets collaborate closely in hemostasis, the process that stops bleeding. Platelets form clots, while certain WBCs aid in repairing the damaged blood vessels.
Initial Response to Injury
Upon injury, platelets rush to the site, forming a clot, while WBCs help fight any invading pathogens and start the healing process.
Collaboration between WBCs and Platelets
This collaboration is essential in inflammation and healing, with WBCs clearing infections and platelets aiding in tissue repair.
Inflammation and Healing
WBCs’ Role in Inflammation
WBCs are key in the inflammatory process, defending against infections and facilitating the body’s healing mechanism.
Platelets in Wound Healing
Beyond clotting, platelets release growth factors that promote tissue repair and regeneration, highlighting their critical role in healing.
Impact of Abnormal Levels
High WBC Count
A high WBC count might indicate an ongoing infection, inflammation, or more severe conditions like leukemia. It can also affect platelet function, influencing the body’s clotting capability.
Low WBC Count
A low WBC count presents significant health risks, such as a higher susceptibility to infections. It can also impact platelet function and the body’s ability to form clots.
High Platelet Count
An elevated platelet count can lead to health issues like thrombosis, where clots form in blood vessels, potentially blocking blood flow. This condition often relates to WBC activity and underlying health conditions.
Low Platelet Count
A low platelet count raises concerns about bleeding risks and can indicate bone marrow problems or autoimmune diseases. It also affects how WBCs function, particularly in response to injury or infection.
Factors Affecting Counts
Medical Conditions
Various diseases, including leukemia, anemia, and autoimmune disorders, directly impact WBC and platelet counts, altering the body’s defense and healing capabilities.
Lifestyle and Environment
Diet, exercise, and exposure to toxins can significantly influence WBC and platelet levels. A healthy lifestyle can support optimal blood cell production and function, while negative environmental factors can lead to detrimental effects.
Diagnostics and Monitoring
Accurate diagnosis and regular monitoring are key to managing the balance between WBCs and platelets effectively. These processes ensure that any abnormalities are caught early and managed appropriately.
Blood Tests
Understanding Complete Blood Count (CBC)
A Complete Blood Count (CBC) is a fundamental blood test that evaluates overall health and detects a range of disorders, including anemia, infection, and leukemia. It measures several components, including:
- Red blood cells (RBCs), which carry oxygen.
- White blood cells (WBCs), which fight infection.
- Platelets, which help with blood clotting.
- Hemoglobin, the oxygen-carrying protein in RBCs.
- Hematocrit, the proportion of RBCs to the fluid component, or plasma, in your blood.
Reading WBC and Platelet Counts
- WBC Count: Normal ranges vary, but generally, a count of 4,500 to 11,000 WBCs per microliter of blood is considered standard. Values outside this range may indicate an underlying condition.
- Platelet Count: A normal platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. Counts outside this range can signify various health issues, from bleeding disorders to thrombotic risks.
Medical Evaluation
When to See a Doctor
You should consider seeing a doctor if you experience symptoms such as unexplained fatigue, weakness, fever, bruising or bleeding more easily than usual. These could be signs of abnormal WBC or platelet counts.
What to Expect During Evaluation
During a medical evaluation, your doctor will:
- Review your medical history and symptoms.
- Perform a physical examination.
- Order a CBC to check your WBC and platelet counts.
- Discuss potential next steps, which might include further testing to identify the cause of any abnormalities.
Treatment and Management
Effective management of abnormal WBC and platelet counts involves both medical interventions and lifestyle modifications, tailored to the specific underlying cause.
Addressing High Counts
Medical Interventions
- For High WBC Count: Treatment may include antibiotics if an infection is the cause, or more specific therapies like chemotherapy for conditions like leukemia.
- For High Platelet Count: Treatment options might involve drugs that reduce platelet production or procedures to remove platelets from the blood.
Lifestyle Modifications
- Maintain a balanced diet rich in fruits, vegetables, and whole grains.
- Exercise regularly, but avoid activities that might cause injury, especially if platelets are high.
- Avoid tobacco and limit alcohol consumption, as these can affect blood cell production.
Managing Low Counts
Treatment Options
- For Low WBC Count: Treatment may involve growth factors to stimulate WBC production or medications to treat the underlying cause.
- For Low Platelet Count: Options include platelet transfusions for severe cases, medications to increase platelet production, or treatments targeting the underlying cause.
Preventative Measures
- Practice good hygiene to reduce the risk of infections, especially important if WBC count is low.
- Avoid activities that increase the risk of bleeding or bruising if platelet counts are low.
- Monitor your health and report any significant changes to your doctor promptly.
FAQs
How do WBCs and platelets interact?
White blood cells and platelets interact in several ways, primarily through signaling molecules that regulate their function and production. For example, during an infection, WBCs can release substances that stimulate platelet activation, enhancing the body’s ability to form clots and trap pathogens. Conversely, activated platelets can release factors that attract and activate WBCs, promoting inflammation and helping to fight infections.
What causes low WBC and platelet counts?
Low counts of WBCs and platelets can result from various conditions, including bone marrow disorders, autoimmune diseases, severe infections, and the side effects of certain medications. These conditions can impair the bone marrow’s ability to produce these cells or lead to their increased destruction in the body.
Can diet and lifestyle affect WBC and platelet levels?
Yes, diet and lifestyle can influence the levels of WBCs and platelets. A balanced diet rich in vitamins and minerals, especially those with antioxidant properties like vitamins C and E, can support the health of the bone marrow and the production of these cells. Regular exercise and avoiding smoking and excessive alcohol consumption can also contribute to maintaining healthy levels of WBCs and platelets.
How are abnormalities in WBC and platelet counts diagnosed?
Abnormalities in WBC and platelet counts are typically diagnosed through blood tests, including a complete blood count (CBC). These tests can identify abnormal levels, which may indicate an underlying condition. Further diagnostic tests, such as bone marrow biopsies, can help determine the cause of these abnormalities.
Conclusion
The complex relationship between white blood cells and platelets underscores the intricate balance necessary for our body’s defense and repair mechanisms. Disruptions in this balance can signal underlying health issues that may require medical attention. It’s essential to understand how these vital components of our blood work together to maintain health and how changes in their levels can affect our overall well-being.
Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can support the optimal function of WBCs and platelets. Awareness and early detection of changes in these blood components can lead to timely intervention, ensuring that our body’s defense and healing systems remain robust and effective.
