Myasthenia Gravis (MG) and Thyroid Disease are two distinct medical conditions, each presenting unique challenges to those affected. While MG is an autoimmune disorder characterized by muscle weakness and fatigue, Thyroid Disease encompasses a range of issues related to the over- or under-functioning of the thyroid gland, affecting metabolism and overall health. Despite their differences, emerging research suggests a fascinating connection between these two conditions, underscoring the intricate ways our immune system and endocrine systems interact.
The relationship between Myasthenia Gravis and Thyroid Disease is grounded in their shared autoimmune nature. Individuals with MG often experience an increased prevalence of thyroid abnormalities, suggesting a complex interplay that can impact diagnosis, treatment, and management strategies. This connection points to the necessity of a careful and integrated approach to healthcare for patients presenting symptoms of either condition.
Exploring the nexus between MG and Thyroid Disease reveals the critical importance of recognizing autoimmune disorders’ systemic nature. It highlights the need for interdisciplinary medical strategies that address the multifaceted aspects of autoimmune diseases and their overlap. By understanding the link between MG and Thyroid Disease, medical professionals can enhance patient care, offering more targeted and effective treatments that consider the potential for concurrent conditions.

Myasthenia Gravis Explained
Definition and Symptoms
Myasthenia Gravis (MG) is a neurological disorder characterized by weakness and fatigue of voluntary muscles. It arises from an autoimmune attack on the communication point between nerves and muscles, known as the neuromuscular junction. Symptoms vary widely among patients but commonly include drooping eyelids, double vision, difficulty swallowing, and general muscle weakness. The severity of these symptoms can fluctuate, often worsening with physical activity and improving with rest.
Causes and Diagnosis
The root cause of MG is the body’s immune system mistakenly attacking the neuromuscular junctions, which prevents muscle cells from receiving signals from the nerve cells. This autoimmune response is believed to be triggered by a combination of genetic and environmental factors, though the exact cause remains elusive. Diagnosing MG involves a combination of clinical evaluation, blood tests for specific antibodies, electromyography (EMG) to assess muscle response, and imaging studies to rule out other conditions.
Treatment Options
Treatment for MG focuses on improving muscle function and involves several strategies:
- Medications such as anticholinesterase agents enhance communication between nerves and muscles, while immunosuppressants reduce the immune system’s attack on the neuromuscular junction.
- Thymectomy, the surgical removal of the thymus gland, is effective in many cases, as the thymus is often abnormal in MG patients.
- Plasmapheresis and intravenous immunoglobulin (IVIg) provide short-term relief during myasthenic crises by removing harmful antibodies from the blood.
Thyroid Disease Uncovered
Types of Thyroid Disease
Thyroid disease encompasses several conditions, all affecting the thyroid gland’s function. The main types are:
- Hypothyroidism, where the thyroid produces insufficient hormones, leading to a slowdown in bodily functions.
- Hyperthyroidism, characterized by excessive thyroid hormone production, speeding up bodily processes.
- Autoimmune thyroid diseases, such as Graves’ disease and Hashimoto’s thyroiditis, where the immune system attacks the thyroid gland.
Symptoms and Effects
Thyroid disease symptoms depend on whether the thyroid is overactive or underactive. Hypothyroidism can lead to fatigue, weight gain, and cold intolerance, while hyperthyroidism may cause weight loss, heat intolerance, and irritability. Both conditions can significantly impact quality of life and require timely diagnosis and management.
Diagnosis and Treatment
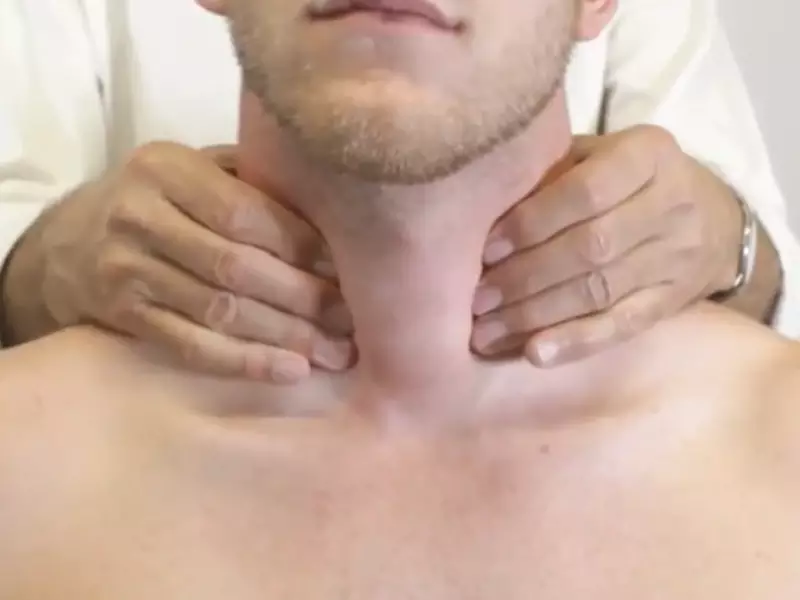
Diagnosis of thyroid disease involves blood tests to measure levels of thyroid hormones and thyroid-stimulating hormone (TSH). Additional tests, such as ultrasound or radioactive iodine uptake, may be used to assess thyroid gland function and structure. Treatment varies by condition:
- Hypothyroidism is typically treated with thyroid hormone replacement therapy.
- Hyperthyroidism management may involve antithyroid medications, radioactive iodine treatment, or thyroid surgery.
Linking MG and Thyroid Disease
Shared Autoimmune Origins
Both MG and certain types of thyroid disease, notably Graves’ disease and Hashimoto’s thyroiditis, are autoimmune disorders. This commonality suggests a shared underlying mechanism, where the immune system mistakenly targets the body’s own tissues – the neuromuscular junction in MG and the thyroid gland in thyroid diseases.
Statistical Connections
Research indicates a higher prevalence of thyroid disorders among patients with MG than in the general population. This association underscores the need for healthcare providers to screen for both conditions when diagnosing either.
Impact of Thyroid Function on MG
Thyroid hormones play a crucial role in energy metabolism and can influence the severity of MG symptoms. Hyperthyroidism may exacerbate muscle weakness, while hypothyroidism can lead to increased fatigue. Managing thyroid disease effectively is therefore paramount in patients with MG to optimize their overall health and quality of life.
Diagnosing Dual Conditions
Challenges in Dual Diagnosis
Diagnosing MG and thyroid disease concurrently presents unique challenges. Symptoms of both conditions can overlap, making it difficult to attribute specific symptoms to one condition over the other. Moreover, the treatment for one disease may complicate the management of the other, necessitating a carefully coordinated approach.
Diagnostic Tests and Indicators
A comprehensive evaluation for patients suspected of having both conditions may include a wide range of tests:
- Blood tests for antibodies related to both MG and thyroid disease.
- Thyroid function tests to assess hormone levels.
- EMG for MG diagnosis.
- Ultrasound of the thyroid gland.
These tests help differentiate between the diseases and guide an effective treatment plan.
Importance of Comprehensive Evaluation
A thorough and comprehensive evaluation is critical for patients presenting with symptoms of both MG and thyroid disease. Accurate diagnosis ensures that treatments do not interfere with each other and are tailored to address both conditions effectively, improving patient outcomes and quality of life.
Treatment and Management
Treating MG and Thyroid Disease Concurrently
Managing both Myasthenia Gravis (MG) and Thyroid Disease simultaneously requires a delicate balance, as treatments for one condition may impact the other. Coordination between neurologists and endocrinologists is essential to create a comprehensive treatment plan that addresses both diseases effectively.
Medication Adjustments and Considerations
MG Treatments
- Anticholinesterase medications enhance communication between nerves and muscles but must be used cautiously if thyroid disease is also present.
- Immunosuppressants can help control the autoimmune aspects of both conditions, yet careful monitoring is necessary to avoid affecting thyroid function.
Thyroid Disease Treatments
- Thyroid hormone replacement therapy is crucial for hypothyroidism management but requires dosage adjustments to avoid exacerbating MG symptoms.
- Antithyroid medications for hyperthyroidism need careful dosing to prevent muscle weakness in MG.
Coordination of Care
- Regular blood tests to monitor medication effects on both conditions.
- Adjusting medication dosages based on symptoms and side effects.
Lifestyle and Dietary Adjustments
For MG
- Rest periods throughout the day to manage fatigue.
- Physical therapy to maintain muscle strength without overexertion.
For Thyroid Disease
- Iodine-rich diet for certain thyroid conditions, balanced with MG dietary recommendations.
- Avoiding excessive soy and cruciferous vegetables, which can interfere with thyroid hormone production and absorption.
General Recommendations
- Regular, moderate exercise that considers both MG and thyroid disease limitations.
- Stress management techniques, as stress can aggravate both conditions.
Patient Stories
Case Studies and Real-Life Experiences
Highlighting patient stories provides invaluable insights into living with MG and Thyroid Disease, showcasing the challenges and successes in treatment and management.
Story 1: Overcoming Fatigue
- A patient with both MG and hypothyroidism describes how adjusting thyroid medication and incorporating regular rest helped manage overwhelming fatigue and muscle weakness.
Story 2: Finding Balance
- Another shares their journey of balancing exercise with rest, and how dietary adjustments improved both their MG symptoms and thyroid function.
Managing Symptoms and Treatment Success
These stories emphasize the importance of personalized treatment plans and the positive impact of patient involvement in their care. Success often comes from trial and error, highlighting the need for open communication with healthcare providers.
Research and Developments
Recent Studies on MG and Thyroid Disease Link
Emerging research continues to explore the connection between MG and Thyroid Disease, offering new insights into their shared autoimmune mechanisms and potential for targeted treatments.
Genetic Factors
- Studies have identified specific genetic markers that may increase susceptibility to both conditions, suggesting a shared pathophysiological basis.
Immunological Insights
- Research into the immune system’s role has led to a better understanding of how autoimmune diseases like MG and Thyroid Disease can coexist and influence each other.
Ongoing Research and Potential Breakthroughs
Novel Therapies
- Ongoing trials of biologic drugs aimed at specific immune system targets offer hope for more effective and less harmful treatments for both conditions.
Personalized Medicine
- Advances in genetic testing and immunotherapy hold the promise of more personalized, effective treatment plans tailored to the individual’s genetic makeup and disease presentation.
Understanding Environmental Triggers
- Investigating how environmental factors contribute to the development of autoimmune diseases could lead to preventive strategies and reduce the incidence of MG and Thyroid Disease.
Frequently Asked Questions
Can Myasthenia Gravis cause Thyroid Disease?
While Myasthenia Gravis itself does not cause Thyroid Disease, the autoimmune nature of MG increases the likelihood of developing other autoimmune disorders, including various forms of Thyroid Disease. Patients with MG are advised to monitor their thyroid function regularly as part of their ongoing care.
How does Thyroid Disease affect Myasthenia Gravis?
Thyroid Disease can exacerbate the symptoms of Myasthenia Gravis, particularly in cases of hyperthyroidism, where excessive thyroid hormone production can lead to increased muscle weakness and fatigue. Proper management of thyroid levels is crucial for individuals with MG to maintain their health and quality of life.
Are there specific treatments for people with both conditions?
Treatment for individuals diagnosed with both Myasthenia Gravis and Thyroid Disease typically involves a coordinated approach to manage both conditions effectively. This may include immunosuppressive therapies for MG and thyroid hormone replacement or suppression for Thyroid Disease, tailored to the individual’s specific needs and response to treatment.
Can thyroid surgery affect Myasthenia Gravis?
Thyroid surgery, particularly in cases of thyroid cancer or severe hyperthyroidism, can impact individuals with Myasthenia Gravis. The stress of surgery and changes in thyroid hormone levels may temporarily worsen MG symptoms. Preoperative and postoperative care must be carefully planned in consultation with both endocrinologists and neurologists.
Conclusion
The intricate relationship between Myasthenia Gravis and Thyroid Disease underscores the complexity of autoimmune disorders and their impact on the human body. This connection not only highlights the importance of an integrated approach to diagnosis and treatment but also points to the need for ongoing research to fully understand and address the interplay between these conditions.
In conclusion, awareness and education on the link between Myasthenia Gravis and Thyroid Disease are crucial. It enables patients and healthcare providers to navigate these challenges more effectively, ensuring a comprehensive care plan that addresses all facets of the patient’s health. As we advance in our understanding, the potential to improve the lives of those affected by these conditions grows, offering hope for more effective treatments and outcomes.
