The kidneys are marvels of biological engineering, tasked with the vital job of filtering blood, removing waste, and balancing bodily fluids. Their intricate processes, tubular reabsorption, and secretion play pivotal roles in maintaining our overall health. Despite their complexity, a basic understanding of these functions can illuminate how our bodies conserve essential nutrients and expel toxins, highlighting the kidneys’ contribution to homeostasis and wellbeing.
Tubular reabsorption and tubular secretion are two distinct processes occurring in the kidneys that manage the body’s fluid and electrolyte balance. Reabsorption is the process by which the kidneys recover water and essential solutes from the filtrate back into the bloodstream, while secretion involves the selective transfer of waste products from the blood into the urinary filtrate. These complementary actions ensure that necessary substances are retained and excesses or toxins are eliminated from the body.
Focusing on these processes reveals the kidneys’ critical role in filtering blood, controlling blood pressure, and regulating electrolyte balance. By precisely adjusting the composition of urine, the kidneys execute a fine balancing act—conserving needed substances while removing unwanted ones. This dynamic interplay not only keeps our internal environment stable but also protects us against a range of health issues, from dehydration to toxic overload.
Kidney Basics
Structure and Function
The kidneys are vital organs located on either side of the spine, just below the rib cage. Their primary role is to filter blood, remove waste products, and balance fluids and electrolytes in the body. Each kidney contains approximately a million filtering units called nephrons, which are the workhorses of the kidneys, ensuring that waste products and excess water are removed from the bloodstream to form urine.
Kidney Anatomy
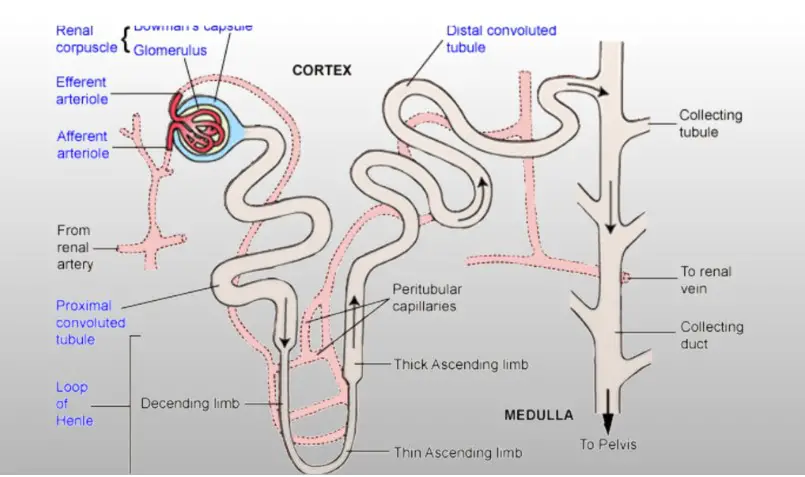
A kidney is roughly the size of a large fist and has a bean-like shape. The outer region of the kidney is called the cortex, and the inner area is the medulla. These areas contain the nephrons, the functional units that filter blood and produce urine. Blood enters the kidney through the renal artery, is filtered through the nephrons, and exits the kidney via the renal vein. The ureter of each kidney then transports the urine to the bladder for excretion.
Role in Homeostasis
The kidneys play a crucial role in maintaining homeostasis—the body’s internal balance. They regulate blood pressure, electrolyte balance, and red blood cell production through the release of hormones. The kidneys also ensure fluid balance in the body, a critical function for all cellular operations and the overall health of an individual.
Nephron: The Functional Unit
Nephron Structure
A nephron begins with a structure called the glomerulus, a tiny blood vessel knot enclosed by a cup-shaped structure known as Bowman’s capsule. This setup initiates the filtration process. The filtered fluid then travels through a coiled tube, the tubule, which reabsorbs essential nutrients and water back into the bloodstream while secreting unwanted substances into the urine.
Importance in Urine Formation
The nephron is essential in the urine formation process. It filters out toxins, excess salts, and urea—a waste product formed through the normal breakdown of proteins. Through a complex process involving filtration, reabsorption, and secretion, nephrons ensure that waste products are excreted while retaining substances vital to the body’s health.
Tubular Reabsorption
Overview
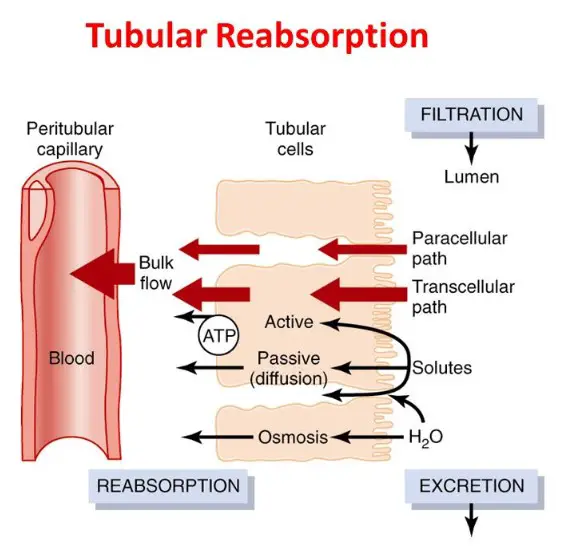
Tubular reabsorption is a critical process whereby the kidneys recover water and solutes from the filtrate (the fluid and dissolved substances that have passed through the glomerulus into Bowman’s capsule) and return them to the blood.
Definition
Tubular reabsorption is the process of moving substances from the renal tubules back into the bloodstream. This process is selective and efficient, ensuring that essential nutrients and a significant amount of water do not go to waste.
Role in Kidney Function
The primary role of tubular reabsorption is to conserve water and essential nutrients that the body needs to function correctly. Without this process, the body would lose excessive amounts of water and nutrients with each urine excretion, leading to dehydration and nutrient deficiencies.
Mechanisms
Passive Transport
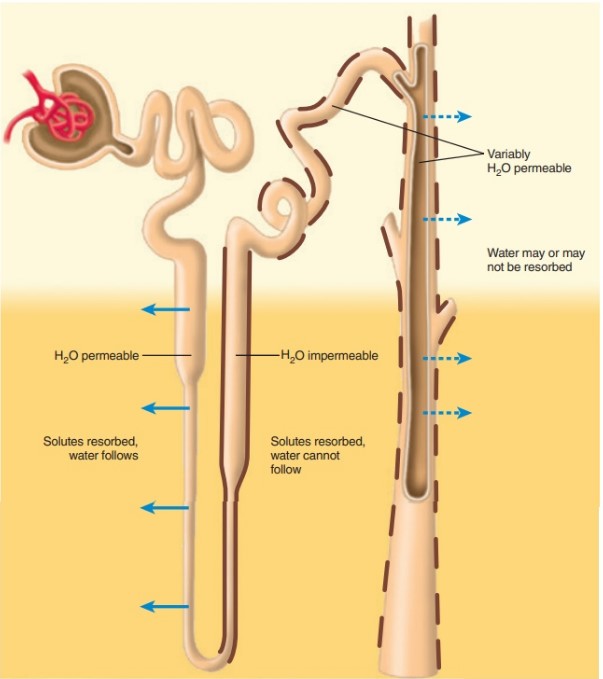
Passive transport occurs when substances move from an area of high concentration to an area of low concentration without the need for energy. This method is mainly used for the reabsorption of water and some ions.
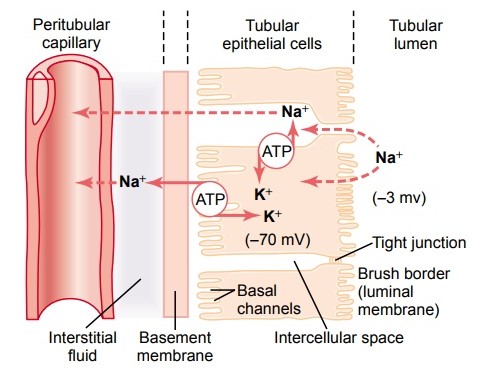
Active Transport
Active transport requires energy to move substances against their concentration gradient. This mechanism is crucial for the reabsorption of glucose, amino acids, and ions such as sodium (Na+), which are transported back into the bloodstream against high concentration gradients.
Osmosis and Diffusion
- Osmosis is the movement of water across a semipermeable membrane from an area of low solute concentration to an area of high solute concentration.
- Diffusion is the passive movement of substances other than water from an area of high concentration to an area of low concentration.
These processes play vital roles in the reabsorption of water and some solutes in the kidney’s nephrons.
Key Substances Reabsorbed
Water
The kidneys reabsorb approximately 90% of the water from the filtrate, preventing dehydration and maintaining fluid balance.
Glucose
Glucose is entirely reabsorbed from the filtrate back into the bloodstream, ensuring that the body retains this vital source of energy.
Ions (Na+, K+, Ca2+)
Ions such as sodium (Na+), potassium (K+), and calcium (Ca2+) are selectively reabsorbed to maintain electrolyte balance and support various bodily functions.
Factors Influencing Reabsorption
Hormonal Regulation (ADH, Aldosterone)
- ADH (Antidiuretic Hormone) increases water reabsorption, reducing urine volume.
- Aldosterone regulates the reabsorption of sodium and potassium, directly influencing blood pressure and fluid balance.
Blood Pressure
Higher blood pressure can increase the filtration rate, affecting the quantities of substances reabsorbed.
Nephron Segment
Different segments of the nephron specialize in reabsorbing specific substances, with the proximal convoluted tubule being notably active in reabsorbing glucose, amino acids, and water.
Tubular Secretion
Overview
Tubular secretion is a crucial renal process that complements tubular reabsorption. While reabsorption focuses on saving valuable substances, secretion is all about removing unwanted materials from the blood. This process helps keep the body’s internal environment stable and healthy by disposing of excess ions, waste products, and toxins through urine.
Definition
Tubular secretion is the selective transfer of substances from the blood into the renal tubular fluid. It’s a targeted method the kidneys use to excrete substances that are too large or too tightly bound to plasma proteins to be filtered through the glomerulus.
Role in Waste Removal
The primary role of tubular secretion is to eliminate waste products and maintain the body’s chemical balance. This includes regulating blood pH by removing excess hydrogen ions and maintaining electrolyte balance by controlling levels of potassium and sodium in the blood.
Mechanisms
Active Transport
Active transport is a key mechanism in tubular secretion, requiring energy to move substances from the blood into the tubular fluid. This is especially important for the secretion of ions and organic acids and bases against their concentration gradient.
Passive Diffusion
Passive diffusion also plays a role, especially in the movement of small, non-ionic substances. This process does not require energy and occurs along the concentration gradient.
Key Substances Secreted
Hydrogen Ions (H+)
The secretion of hydrogen ions is crucial for maintaining the body’s acid-base balance, helping to neutralize the pH of blood and urine.
Potassium Ions (K+)
Potassium is carefully regulated through secretion to prevent hyperkalemia, a condition of elevated potassium levels that can be life-threatening.
Urea and Creatinine
Although primarily eliminated through glomerular filtration, some urea and creatinine are also secreted to ensure their effective removal from the body.
Factors Influencing Secretion
Blood pH
The body’s need to maintain a stable pH influences the rate of hydrogen ion secretion, with increased secretion in acidic conditions to restore balance.
Potassium Levels
The secretion of potassium is closely regulated in response to dietary intake and overall body levels to prevent disturbances in heart and muscle function.
Toxins and Medications
The kidneys play a key role in excreting drugs and toxins, often through active secretion, to protect the body from potential harm.
Comparative Analysis
Similarities and Differences
Process Location
While both processes occur within the nephron, reabsorption mainly takes place in the proximal convoluted tubule, and secretion occurs in the distal convoluted tubule and collecting duct.
Direction of Movement
Reabsorption moves substances from the tubular fluid back into the blood, whereas secretion moves substances from the blood into the tubular fluid.
Substances Involved
Reabsorption focuses on valuable substances like glucose, amino acids, and water. In contrast, secretion targets the elimination of waste products and excess ions.
Physiological Importance
Maintaining Blood pH
Both processes contribute to acid-base balance; reabsorption conserves bicarbonate ions, while secretion removes excess hydrogen ions.
Electrolyte Balance
Reabsorption and secretion together ensure the body maintains the correct levels of essential electrolytes, like sodium, potassium, and calcium.
Blood Pressure Regulation
By controlling the reabsorption of water and sodium, the kidneys influence blood volume and pressure, vital for overall cardiovascular health.
Pathological Conditions
Effects of Impaired Reabsorption or Secretion
Disruptions in these processes can lead to a variety of health issues, including electrolyte imbalances, acidosis or alkalosis, and hypertension.
Kidney Stones
An imbalance in calcium, oxalate, and phosphate reabsorption can lead to the formation of kidney stones, causing pain and potentially blocking urine flow.
Chronic Kidney Disease
Impaired kidney function affects both reabsorption and secretion, leading to the accumulation of toxins and waste in the blood, eventually resulting in chronic kidney disease (CKD).
Frequently Asked Questions
What is tubular reabsorption?
Tubular reabsorption is a vital kidney function where essential nutrients, water, and electrolytes are absorbed back into the bloodstream from the filtered fluid that passes through the renal tubules. This selective process ensures that the body retains necessary substances, such as glucose, amino acids, and ions, preventing their loss through urine and maintaining the body’s internal balance.
How does tubular secretion differ from reabsorption?
Tubular secretion is the process by which the kidneys add certain substances from the blood into the urine. This mechanism serves to remove excess ions, waste products, and drugs from the body, complementing the filtering function of the glomeruli. Unlike reabsorption, which conserves valuable nutrients, secretion focuses on waste elimination and homeostatic regulation of blood pH and electrolyte levels.
Why are these processes important for maintaining health?
Tubular reabsorption and secretion are essential for maintaining fluid and electrolyte balance, regulating blood pressure, and ensuring the removal of metabolic wastes and toxins. Disruptions in these processes can lead to serious health issues, including electrolyte imbalances, hypertension, and kidney disease. Understanding these functions is crucial for recognizing how the kidneys support overall health and how disruptions can impact bodily systems.
Conclusion
The kidneys’ roles in tubular reabsorption and secretion underscore their critical importance in maintaining the delicate balance of our body’s internal environment. By efficiently managing the retention of nutrients and the elimination of wastes, these processes exemplify the body’s sophisticated mechanisms for sustaining life. Appreciating the complexity and precision of kidney functions not only deepens our understanding of human physiology but also highlights the significance of maintaining kidney health for overall wellbeing.
Recognizing the intricacies of tubular reabsorption and secretion offers a window into the body’s remarkable capacity to self-regulate and maintain homeostasis. It reminds us of the vital importance of kidney health, encouraging proactive measures to support these essential organs. In doing so, we safeguard our health, ensuring that the body’s internal harmony is preserved against the challenges of diseases and environmental factors.