Nutritional support is a pivotal aspect of medical care for patients unable to meet their nutritional needs due to illness, surgery, or other health conditions. The provision of nutrients directly into the bloodstream or the gastrointestinal tract plays a critical role in patient recovery and overall health. This article focuses on the two primary methods of delivering such support: Total Parenteral Nutrition (TPN) and Tube Feeding.
The main difference between TPN and Tube Feeding lies in the method of delivery and the target system for nutrient absorption. TPN bypasses the digestive tract entirely, delivering nutrients directly into the bloodstream, while Tube Feeding involves delivering nutrition into the stomach or intestine, utilizing the digestive system for nutrient absorption.
Nutritional support strategies like TPN and Tube Feeding are chosen based on the specific needs and conditions of the patient. Each method has its indications, benefits, and risks, making the decision a critical component of patient care. The choice between TPN and Tube Feeding depends on several factors including the patient’s gastrointestinal function, risk of infection, and long-term nutritional needs.
What is TPN?
Definition and Purpose
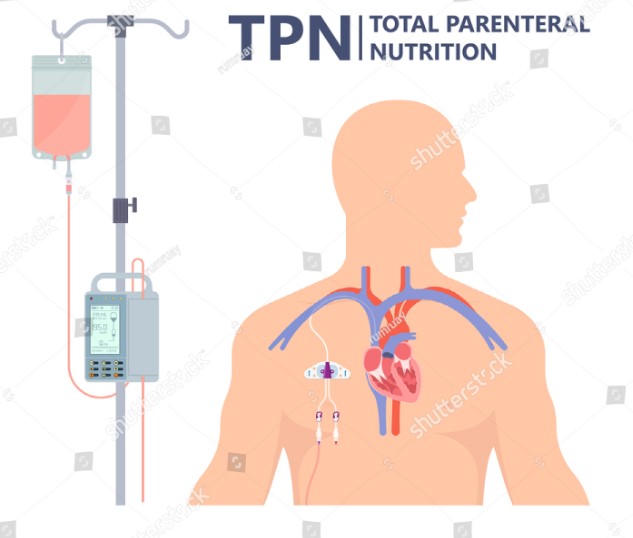
Total Parenteral Nutrition (TPN) is a method of feeding that bypasses the gastrointestinal tract, directly delivering nutrients into the bloodstream through an intravenous (IV) line. The primary purpose of TPN is to ensure that patients who cannot use their digestive system still receive the necessary nutrition to recover, maintain, or improve their health.
How TPN Works
TPN works by providing a complete nutritional formula that includes carbohydrates, proteins, fats, vitamins, and minerals, directly into a patient’s circulatory system. This process involves:
- Inserting a central line or a peripherally inserted central catheter (PICC) into a large vein, typically in the chest or arm.
- Administering the nutritional formula through this line, which is absorbed directly by the body’s cells.
Components of TPN
The components of TPN are designed to mimic the nutritional value of a complete diet and can be tailored to meet the specific needs of each patient. These components include:
- Carbohydrates, typically in the form of glucose, provide energy.
- Proteins (amino acids) for cell growth and repair.
- Fats (lipids) for energy and cell function.
- Vitamins and minerals to ensure the body functions properly.
- Electrolytes to maintain nerve and muscle function, hydration, blood pH, and to rebuild damaged tissues.
What is Tube Feeding?
Definition and Purpose
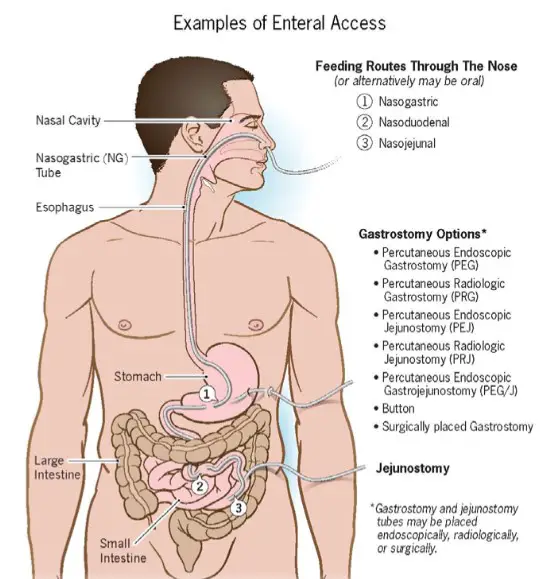
Tube Feeding, also known as enteral nutrition, involves delivering a liquid nutrition formula directly into the stomach or small intestine through a tube. This method is used when a person can digest and absorb nutrients but cannot ingest food orally due to various reasons like surgery, injury, or illness.
Types of Tube Feeding
There are several types of tube feeding, depending on the insertion site and the patient’s needs:
- Nasogastric (NG) Tube: Runs from the nose to the stomach.
- Nasojejunal (NJ) Tube: Extends from the nose to the jejunum (part of the small intestine).
- Gastrostomy (G) Tube: Inserted directly into the stomach through the abdominal wall.
- Jejunostomy (J) Tube: Placed directly into the small intestine through the abdominal wall.
Components of Enteral Formulas
The enteral formulas used in tube feeding vary based on the patient’s nutritional requirements but generally include:
- Macronutrients: Carbohydrates, proteins, and fats.
- Micronutrients: Vitamins and minerals.
- Specialized formulas are available for patients with specific needs, such as kidney disease, liver disease, or diabetes.
Key Differences
Nutrition Delivery Method
- TPN delivers nutrition directly into the bloodstream, bypassing the digestive system entirely.
- Tube Feeding utilizes the digestive tract by delivering nutrition directly to the stomach or intestine.
Indications for Use
- TPN is indicated for patients with non-functional or severely impaired gastrointestinal tracts.
- Tube Feeding is suitable for patients who are unable to consume adequate nutrition orally but have a partially or fully functional gastrointestinal tract.
Risk and Complications
- TPN carries risks such as infections, liver complications, and nutrient imbalances.
- Tube Feeding may lead to gastrointestinal complications like diarrhea, constipation, and tube displacement.
Indications for TPN
TPN is recommended when the digestive system is not in a state to process or absorb nutrients effectively. Conditions that may require TPN include:
- Severe gastrointestinal diseases (e.g., Crohn’s disease, short bowel syndrome).
- Major abdominal surgery recovery.
- Certain types of cancer and cancer treatments that impair digestion or absorption.
Indications for Tube Feeding
Tube Feeding is advised for patients who:
- Have difficulty swallowing due to neurological or muscular disorders.
- Are unable to ingest enough nutrition orally.
- Have conditions like stroke, head injury, or esophageal disorders which affect the normal intake of food.
Procedure Comparison
TPN Administration Process
Total Parenteral Nutrition (TPN) is a complex medical process designed for patients who cannot digest or absorb nutrients through their gastrointestinal tract. Here’s how TPN administration typically works:
- Assessment: A healthcare professional assesses the patient’s nutritional needs based on their medical condition, weight, and nutritional requirements.
- Catheter Placement: A central line or catheter is placed into a large vein, usually in the chest or arm, through which nutrients are delivered.
- Nutrient Preparation: A pharmacist or a trained specialist prepares the TPN solution, tailored to the patient’s specific nutritional needs.
- Administration: The TPN solution is administered through the catheter using a pump, ensuring a controlled and steady flow of nutrients.
Tube Feeding Administration Process
Tube feeding, also known as enteral nutrition, involves the delivery of nutrients directly into the stomach or intestine. The process includes:
- Tube Placement: Depending on the type, a tube is placed either through the nose to the stomach (nasogastric) or directly into the stomach or intestine through the skin (gastrostomy or jejunostomy).
- Formula Selection: A healthcare provider selects an enteral formula that matches the patient’s nutritional needs and medical condition.
- Feeding Schedule: Feedings are scheduled at regular intervals, either as continuous infusions or bolus feedings, depending on the patient’s tolerance.
Risks and Complications
TPN-Associated Risks
While TPN is life-saving, it carries certain risks:
- Infection: The central line can become a gateway for bacteria, leading to serious infections.
- Liver Problems: Long-term TPN use can affect liver function.
- Metabolic Imbalances: Imbalances in electrolytes and glucose levels can occur, necessitating close monitoring.
Tube Feeding-Associated Risks
Tube feeding is generally safer but not without risks:
- Aspiration: There’s a risk of food entering the lungs, leading to pneumonia.
- Tube Displacement: The feeding tube may move or get dislodged.
- Digestive Issues: Diarrhea, constipation, and bloating can affect patients.
Nutritional Content
TPN solutions are customized, containing all necessary nutrients: carbohydrates, proteins, fats, vitamins, minerals, and trace elements. They are designed to meet the complete nutritional needs of the patient intravenously.
Tube feeding formulas also offer a complete range of nutrients but are designed to be digested and absorbed by the gastrointestinal tract. They come in various forms, including fiber-containing formulas, disease-specific formulas, and standard formulas.
Monitoring and Management
Monitoring for TPN
Regular blood tests monitor electrolyte levels, liver and kidney function, and blood glucose levels. Monitoring helps in adjusting the nutrient composition of the TPN solution to meet the changing needs of the patient.
Monitoring for Tube Feeding
For tube feeding, monitoring includes checking the tube placement, digestive tolerance, and ensuring that the patient is receiving adequate nutrition. Signs of intolerance like nausea, vomiting, and abdominal distension are closely observed.
Adjustments and Management Strategies
Both TPN and tube feeding require adjustments based on the patient’s response:
- Nutrient Adjustments: Tailoring the nutrient composition to address deficiencies or excesses.
- Method Adjustments: Transitioning from TPN to tube feeding or oral intake as the patient’s condition improves.
Cost Considerations
TPN is significantly more expensive due to the need for sterile equipment, specialized formulations, and close medical monitoring. Tube feeding is less costly, with expenses primarily around the feeding formulas and equipment. The choice between TPN and tube feeding can significantly impact healthcare decisions, especially in long-term care settings.
Patient Quality of Life
TPN and tube feeding can affect a patient’s quality of life in different ways. TPN requires dealing with a central line, which can restrict movement and activities, while tube feeding might affect self-image and social interactions. Psychological support and counseling are important for patients and their families.
Case Studies
TPN Use
A case study of a patient with severe Crohn’s disease, unable to absorb nutrients through the GI tract, showed remarkable recovery on TPN, highlighting the importance of personalized nutritional support.
Tube Feeding Use
Another case involved an elderly patient recovering from stroke-related dysphagia. Tube feeding supported nutritional needs until gradual reintroduction to oral feeding, showcasing the potential for recovery and transition.
FAQs
What is Total Parenteral Nutrition?
Total Parenteral Nutrition (TPN) is a method of feeding that bypasses the digestive tract, delivering nutrients directly into the bloodstream. It’s used for patients who cannot or should not receive feedings or fluids by mouth or tube feeding. TPN provides all the necessary nutrients such as carbohydrates, proteins, fats, vitamins, and minerals.
When is Tube Feeding Recommended?
Tube Feeding is recommended for patients who are unable to meet their nutritional needs by oral intake but have a functioning gastrointestinal tract. Conditions such as neurological disorders, gastrointestinal diseases, and severe swallowing disorders often necessitate the use of tube feeding to ensure adequate nutrition.
How are TPN and Tube Feeding Monitored?
The monitoring of TPN involves regular blood tests to ensure that the nutrients are being absorbed properly and to prevent complications such as infections or liver problems. Tube Feeding monitoring focuses on digestive system response, ensuring the proper absorption of nutrients, and watching for any signs of intolerance or blockage.
Can TPN and Tube Feeding be Used Concurrently?
TPN and Tube Feeding are typically not used concurrently as they serve different purposes based on the patient’s ability to digest and absorb nutrients. However, in certain transition phases or specific medical conditions, a patient might receive both methods in a carefully monitored approach to meet their nutritional requirements.
Conclusion
The decision between Total Parenteral Nutrition (TPN) and Tube Feeding is a significant one, influenced by a patient’s specific medical conditions, nutritional needs, and overall health goals. While TPN is essential for individuals whose digestive systems are not functional, Tube Feeding offers a solution for those who can use their gastrointestinal tract but cannot achieve adequate nutrition orally.
In conclusion, understanding the key differences between TPN and Tube Feeding, their applications, risks, and benefits, is crucial for optimizing patient care. This knowledge ensures that patients receive the most appropriate form of nutritional support, tailored to their unique health needs, thus enhancing recovery and improving quality of life.