The human body is a complex network of structures and systems, where each component plays a critical role in maintaining overall health. Among these, the spermatic cord and inguinal canal are key structures located within the lower abdominal region. Their functions and relevance in male physiology are often topics of detailed study in medical science.
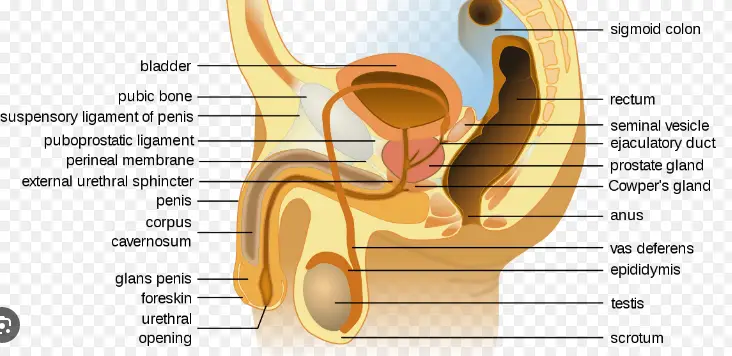
The spermatic cord, essentially a bundle of fibers and tissues, encapsulates vital elements including arteries, veins, nerves, and the ductus deferens. Meanwhile, the inguinal canal, positioned at the lower abdomen, acts primarily as a passageway for the spermatic cord and, in women, the round ligament of the uterus. This canal is crucial in both genders for different reasons, predominantly in relation to the groin and reproductive organs.
These structures are not just anatomical entities; they hold significant clinical importance due to their roles and the common medical conditions associated with them. From hernias to pain syndromes, understanding these parts of the body helps in diagnosing, treating, and preventing various health issues.
Anatomy Overview
The human body hosts a myriad of anatomical structures that are essential for proper physiological functioning. Among these, the spermatic cord and inguinal canal play crucial roles, particularly in the male reproductive system and general abdominal health.
What is the Spermatic Cord?
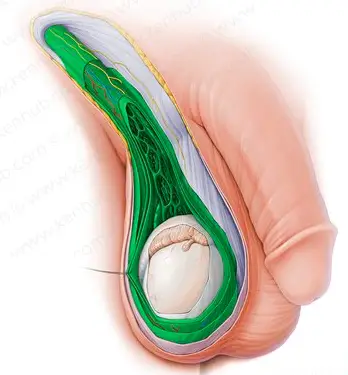
The spermatic cord is an essential structure in male anatomy, particularly involved in reproductive and sexual health. It is a cord-like collection of fibers and tissues that extends from the deep inguinal ring down to the testicles. Here’s what it contains:
- Arteries (testicular artery) that supply blood to the testes.
- Veins (pampiniform plexus) that help drain blood from the testes.
- Lymphatic vessels that are responsible for draining lymph.
- Nerves (such as the genital branch of the genitofemoral nerve) that provide sensation.
- The vas deferens, which is the duct that carries sperm from the testicle to the urethra.
What is the Inguinal Canal?
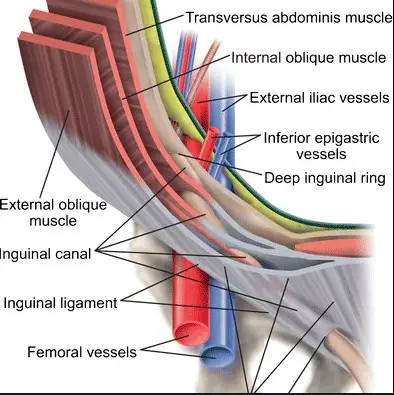
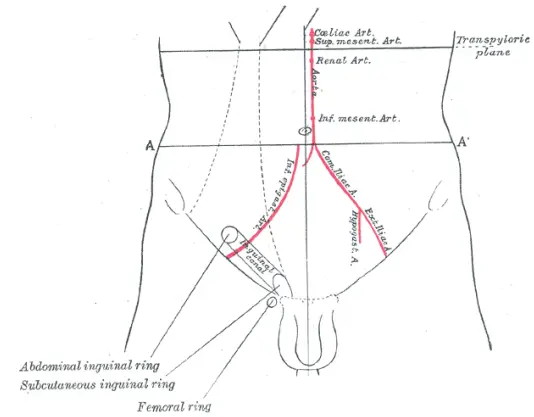
The inguinal canal is another significant structure located in the lower abdomen, just above the inguinal ligament. It is crucial in both sexes but serves different functions:
- In males, it allows the spermatic cord to pass from the abdomen to the scrotum.
- In females, it contains the round ligament of the uterus, supporting the womb.
This canal is formed by layers of abdominal muscles which create a natural passageway. It starts from the deep inguinal ring within the abdomen and extends to the superficial inguinal ring at the pubic region.
Comparative Anatomy
Understanding the differences and similarities between the spermatic cord and inguinal canal is key to grasping their functions and clinical significance.
Physical Location Differences
- Spermatic Cord: Begins at the deep inguinal ring, descends through the inguinal canal, and ends in the scrotum.
- Inguinal Canal: Located at the front part of the lower abdomen, stretching from the deep inguinal ring to the superficial inguinal ring.
Structural Components
The structures of the spermatic cord and the inguinal canal, while interconnected, have distinct components that define their anatomy:
- The spermatic cord is mainly composed of vessels, nerves, and the vas deferens, wrapped together in a sheath of fascia.
- The inguinal canal, however, is defined by the muscular and fascial layers of the abdomen, forming a canal-like structure that houses the spermatic cord or the round ligament in females.
Functions
Both the spermatic cord and inguinal canal have vital roles in bodily functions, especially concerning reproductive health and abdominal integrity.
Role of the Spermatic Cord
The spermatic cord has several key functions:
- Temperature regulation: The pampiniform plexus, a network of veins within the cord, helps regulate the temperature of the testes which is crucial for optimal sperm production.
- Transportation: It acts as a conduit for sperm through the vas deferens from the testicles to the urethra.
Role of the Inguinal Canal
The inguinal canal, while primarily a structural passage, also serves important roles:
- Structural support: It provides a pathway that helps maintain the structural integrity of the lower abdominal wall.
- Facilitates movement: In females, the round ligament which runs through the inguinal canal helps stabilize the uterus.
Clinical Significance
The spermatic cord and inguinal canal are not only critical in terms of anatomy and function but also in clinical settings. Their involvement in various medical conditions makes understanding these structures important for diagnosing and managing specific health issues.
Health Issues Involving Spermatic Cord
Several conditions can affect the spermatic cord, each presenting unique challenges in the medical field:
- Testicular torsion: This acute and painful condition occurs when the spermatic cord twists, cutting off blood supply to the testicles. It requires immediate surgical intervention to prevent testicular death.
- Varicocele: A varicocele is an enlargement of the veins within the pampiniform plexus of the spermatic cord. Commonly described as feeling like a “bag of worms,” this condition can cause pain and lead to infertility.
- Infections: Epididymitis, an infection of the epididymis that can spread to the spermatic cord, often results in pain and swelling. It’s typically treated with antibiotics.
These conditions highlight the necessity for awareness and timely intervention, as they can have significant repercussions on reproductive and general health.
Health Issues Involving Inguinal Canal
The inguinal canal, while primarily a passageway, is also prone to several disorders:
- Inguinal hernias: The most common issue associated with the inguinal canal is an inguinal hernia, where abdominal contents protrude through a weak spot in the groin muscles. These hernias can be painful and may require surgical repair to prevent complications.
- Hydrocele and hernia in infants and children: Congenital issues such as hydroceles and hernias can manifest in newborns, involving the inguinal canal. These typically resolve on their own or with minor surgery.
Surgical Insights
Given their clinical significance, both the spermatic cord and inguinal canal are frequently involved in surgical procedures. Understanding the surgical approaches to these structures is crucial for medical professionals.
Surgery on the Spermatic Cord
Surgical interventions on the spermatic cord are often performed to correct conditions such as varicoceles and testicular torsion:
- Varicocelectomy: This procedure involves the ligation of the abnormally dilated veins to alleviate pain and restore proper blood flow, potentially improving fertility.
- Orchiopexy for testicular torsion: This surgery aims to untwist the spermatic cord and secure the testicles to the scrotum to prevent future torsion.
Surgery on the Inguinal Canal
Inguinal canal surgeries are predominantly performed to repair hernias:
- Open hernia repair: This traditional method involves making a large incision in the groin area to push the protruding tissue back into place and strengthen the abdominal wall with stitches or mesh.
- Laparoscopic hernia repair: A minimally invasive approach that uses small incisions, a camera, and surgical tools to repair the hernia, often resulting in quicker recovery and less pain post-operation.
Step-by-Step Guide to Hernia Surgery
Here’s a simplified overview of what happens during a typical laparoscopic hernia repair procedure:
- Preparation: The patient is placed under general anesthesia.
- Incision: Several small incisions are made in the abdomen.
- Insertion of laparoscope: A laparoscope, which is a thin tube with a camera at the end, is inserted through one of the incisions.
- Repair: Surgical instruments are used through other incisions to repair the hernia with synthetic mesh.
- Closure: The incisions are closed with sutures or surgical glue.
FAQs
What is the Spermatic Cord?
The spermatic cord is an assembly of blood vessels, nerves, and the vas deferens that run through the abdominal region to the testicles. It’s vital for providing blood flow and regulating the temperature of the testes, which is crucial for sperm production and overall reproductive health.
What is the Inguinal Canal?
The inguinal canal is an anatomical passage in the lower abdomen, important for males and females. In males, it allows the spermatic cord to pass to the testicles, and in females, it transmits the round ligament of the uterus. This canal is a common site where inguinal hernias can occur, especially in men.
How do the Spermatic Cord and Inguinal Canal differ?
While the inguinal canal serves as a passage, the spermatic cord is a content within this canal in males. Structurally, the inguinal canal is a pathway that includes muscular and fascial layers, whereas the spermatic cord comprises vessels, nerves, and the vas deferens bundled together by fascia.
Why are these structures clinically significant?
Both structures are pivotal in understanding certain common and complex medical conditions like hernias. The integrity of the inguinal canal is crucial to prevent hernias, while issues with the spermatic cord can lead to pain or complications in fertility.
Conclusion
In summarizing the significance of the spermatic cord and inguinal canal, it is clear that both play pivotal roles in bodily functions, particularly in the reproductive and structural integrity of the lower abdomen. Their study and understanding are indispensable in the fields of anatomy and medicine.
The importance of these anatomical features extends beyond their biological roles, as they are often central in various clinical scenarios. Effective treatment of conditions related to these structures can lead to improved outcomes in patient health, showcasing the critical need for awareness and knowledge in these areas.