The male reproductive system comprises various specialized structures and cell types, each with critical roles in reproduction. Among these, seminiferous tubules and Leydig cells are integral components, essential for sperm production and hormone secretion, respectively. These elements not only define the functional landscape of the testes but also highlight the complexity of reproductive biology.
Seminiferous tubules are the sites where sperm cells are produced, a process known as spermatogenesis. Leydig cells, located between the tubules, are responsible for producing testosterone, the hormone crucial for male sexual development and reproductive function. The key difference between these two lies in their primary functions and locations within the testes.
While seminiferous tubules focus on sperm production, Leydig cells are chiefly involved in hormonal regulation, underlining a division of labor within the testes that ensures efficient reproductive health. Understanding their structural and functional differences is vital for insights into male fertility and the diagnosis and treatment of related disorders.
Seminiferous Tubules Overview
Definition and Function
Seminiferous tubules are specialized structures within the male reproductive organs, specifically located in the testes. These tubules are the sites where sperm production, or spermatogenesis, occurs. The primary function of these tubules is not only to produce sperm but also to support their development from spermatogonia (sperm precursor cells) to mature spermatozoa, ready for ejaculation.
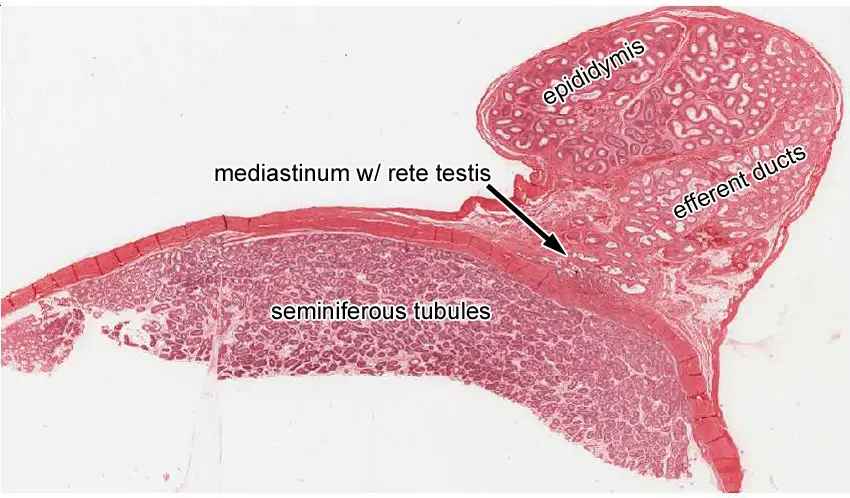
Location and Structure Details
Seminiferous tubules are coiled networks nestled within the testes. Each testis contains about 250-300 tubules, each tubule measuring up to 70 centimeters in length when uncoiled. They are surrounded by a basement membrane and are lined with spermatogenic cells which develop into sperm over several stages. Supporting these cells are Sertoli cells, which nourish the developing sperm and regulate the process by chemical signaling.
Leydig Cells Explained
Definition and Role
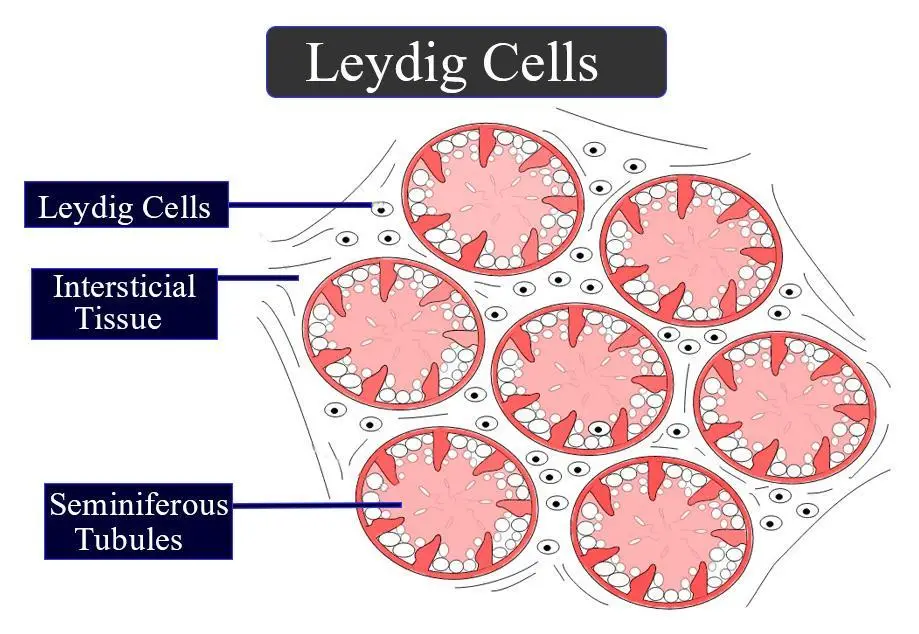
Leydig cells, also known as interstitial cells, are located in the interstitial space between the seminiferous tubules within the testes. Their main role is the production of testosterone, the hormone pivotal for male sexual development and reproductive function. Testosterone influences various bodily functions, from muscle mass and bone density to the regulation of libido and mood.
Location within the Testes
These cells are strategically positioned to quickly respond to hormonal signals and to efficiently deliver testosterone directly into the bloodstream. The proximity of Leydig cells to the blood vessels enhances this process, facilitating rapid effects of testosterone on the body.
Structural Differences
Physical Layout in the Testes
While seminiferous tubules form a convoluted network designed to maximize space for sperm production, Leydig cells fill the spaces between these tubules. This structural arrangement ensures that testosterone produced by the Leydig cells can easily reach the tubules to influence spermatogenesis.
Cellular Composition Comparison
The cellular makeup of seminiferous tubules and Leydig cells distinctly differs. Seminiferous tubules are composed primarily of developing sperm cells and Sertoli cells that provide structural and nutritional support. In contrast, Leydig cells are singular in function and form, focused on hormone synthesis without the complexity of supporting multiple cell types or stages of development.
Functional Variations
Role in Hormone Production
Leydig cells’ primary function is to secrete testosterone in response to luteinizing hormone (LH) from the pituitary gland. This hormone regulation is critical for maintaining male secondary sexual characteristics and overall reproductive health.
Contribution to Spermatogenesis
While Leydig cells manage hormone production, seminiferous tubules are directly involved in the creation and maturation of sperm. This includes multiple stages of cell division and transformation, from spermatogonia to the final spermatozoon. This process is tightly regulated by hormones, including testosterone, which is provided by the Leydig cells.
Interaction and Regulation
How They Work Together
Seminiferous tubules and Leydig cells exhibit a synergistic relationship crucial for the proper functioning of the male reproductive system. This interaction primarily involves the hormonal signals that regulate spermatogenesis and testosterone production. Leydig cells produce testosterone in response to luteinizing hormone (LH), which is then used to assist the process of sperm maturation in the seminiferous tubules. Additionally, Sertoli cells within the tubules produce inhibin, which helps regulate the secretion of follicle-stimulating hormone (FSH) from the pituitary gland.
Hormonal Regulation Impacting Both
Hormonal regulation is vital for the coordination of functions between seminiferous tubules and Leydig cells. The main hormones involved include:
- Luteinizing Hormone (LH): Stimulates Leydig cells to produce testosterone.
- Follicle-Stimulating Hormone (FSH): Acts on Sertoli cells to promote sperm maturation.
- Testosterone: Produced by Leydig cells, it is crucial for the development of male secondary sexual characteristics and spermatogenesis.
- Inhibin: Produced by Sertoli cells, it provides feedback to the pituitary gland to regulate FSH levels.
This hormonal interplay ensures that sperm production and testosterone levels are maintained within optimal ranges to support fertility and overall male health.
Research and Studies
Key Studies on Seminiferous Tubules
Recent studies on seminiferous tubules have focused on understanding the cellular mechanisms that drive spermatogenesis. Research has demonstrated that the microenvironment within these tubules, particularly the role of Sertoli cells, is crucial for the health and viability of sperm cells. Innovations in microscopy and cellular biology have allowed scientists to observe these processes in unprecedented detail, leading to better understanding and potential therapeutic targets for infertility.
Significant Findings on Leydig Cells
Leydig cells have been the subject of numerous studies due to their role in testosterone production. Significant research has shown that Leydig cell function can be affected by various factors, including age, environmental toxins, and lifestyle. For instance, studies have linked certain pesticides and chemicals to decreased Leydig cell efficiency, which correlates with reduced testosterone levels and potential reproductive issues.
Clinical Relevance
Implications in Health and Disease
The health of seminiferous tubules and Leydig cells is paramount in the context of male reproductive health. Disorders in either can lead to serious conditions such as:
- Infertility: Issues in either sperm production or hormone secretion can lead to challenges in conceiving naturally.
- Hypogonadism: This condition, characterized by low testosterone levels, can result from Leydig cell dysfunction.
- Testicular Cancer: Changes in the structure or function of the seminiferous tubules can sometimes indicate or lead to oncogenic processes.
Understanding the implications of tubule and Leydig cell health helps in early diagnosis and management of these conditions.
Treatments Targeting These Structures
Advancements in medical research have led to targeted treatments that address specific dysfunctions in seminiferous tubules and Leydig cells:
- Hormone Replacement Therapy (HRT): Used primarily for treating hypogonadism by supplementing testosterone levels.
- Selective Estrogen Receptor Modulators (SERMs): Used to manage and stimulate testosterone production, which can indirectly support spermatogenesis.
- Antioxidants and Lifestyle Changes: Studies suggest that dietary antioxidants can protect Leydig cells and seminiferous tubules from oxidative stress, thereby improving their function.
Frequently Asked Questions
What are Seminiferous Tubules?
Seminiferous tubules are tightly coiled structures within the testes where sperm cells are produced. These tubules provide the necessary environment for the maturation and development of sperm through the process of spermatogenesis.
What are Leydig Cells?
Leydig cells, also known as interstitial cells, are found adjacent to the seminiferous tubules in the testes. They play a critical role in producing testosterone, the primary male sex hormone, which is essential for sexual development and reproductive function.
How do Seminiferous Tubules and Leydig Cells Interact?
The interaction between seminiferous tubules and Leydig cells is crucial for male reproductive health. Leydig cells produce testosterone, which in turn helps regulate spermatogenesis within the seminiferous tubules, showcasing a symbiotic relationship necessary for sperm production and hormonal balance.
What Affects the Function of Leydig Cells and Seminiferous Tubules?
Various factors can impact the function of Leydig cells and seminiferous tubules, including hormonal imbalances, age, environmental toxins, and certain medical conditions such as hypogonadism or testicular cancer, which can disrupt their normal functioning and affect fertility.
Conclusion
Seminiferous tubules and Leydig cells are pivotal to the male reproductive system, each playing distinct but interrelated roles in spermatogenesis and hormone production. Their collaboration ensures the proper development of male sexual characteristics and fertility, which is fundamental to reproductive health.
The comprehension of these structures not only enriches our understanding of male biology but also aids in the advancement of treatments for reproductive issues. By exploring the differences and interactions between these cell types, medical professionals can better diagnose and treat conditions that impair male reproductive capabilities.