Post-traumatic stress disorder (PTSD) and Complex PTSD (C-PTSD) represent two facets of psychological distress stemming from exposure to traumatic events. While they share common ground in their origins, the nuances between them paint a picture of trauma’s multifaceted impact on the human psyche. These conditions underscore the brain’s response to overwhelming stress, revealing the intricate ways in which prolonged exposure to trauma can affect individuals differently.
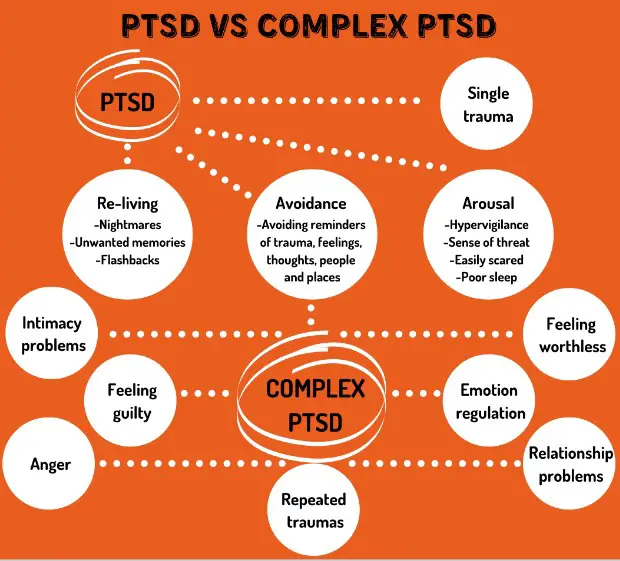
PTSD is a mental health condition triggered by experiencing or witnessing a terrifying event, characterized by flashbacks, severe anxiety, and uncontrollable thoughts about the trauma. In contrast, Complex PTSD results from prolonged exposure to traumatic circumstances, often involving harm or abandonment by a caregiver or interpersonal relationships, leading to more severe and persistent symptoms beyond those of PTSD. This differentiation is crucial for understanding the varied impacts of trauma and the approaches required for healing.
Recognizing the distinction between PTSD and Complex PTSD is essential for both clinical practice and public awareness. It not only facilitates the accurate diagnosis and treatment of those affected but also deepens our understanding of trauma’s complex nature. This insight is pivotal in guiding survivors on their journey towards recovery, emphasizing the importance of specialized support and interventions tailored to the unique challenges they face.
PTSD Explained
Definition and Causes
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after a person experiences or witnesses a traumatic event. These events may include accidents, natural disasters, war, physical assaults, or any situation where one’s life or safety is threatened. The root of PTSD lies in the brain’s response to overwhelming stress, impacting an individual’s ability to cope with and process their experiences.
Psychological trauma and PTSD
Psychological trauma occurs when a person faces events that cause intense fear, helplessness, or horror. The brain can become overwhelmed, and its normal processing mechanisms may not fully process the trauma, leading to long-term stress reactions. This disruption in processing can cause PTSD, where the trauma continually affects the person’s mental health and well-being.
Common triggers
Triggers for PTSD are as varied as the individuals affected by it. However, some common scenarios include:
- Military combat
- Serious accidents
- Violent personal assaults (such as rape)
- Natural or human-caused disasters
- Terrorist attacks
- Witnessing a death or serious injury
Symptoms
The symptoms of PTSD can be grouped into four main categories: intrusive thoughts, avoidance behaviors, negative changes in thinking and mood, and changes in physical and emotional reactions.
Emotional and physical signs
Emotional signs include:
- Flashbacks and nightmares where the traumatic event is relived
- Severe anxiety and hyperarousal
- Depression or feelings of hopelessness
- Irritability or anger
Physical signs might involve:
- Sleep disturbances
- Fatigue
- Being easily startled
- Physical reactions to reminders of the trauma, such as sweating or a racing heart
Impact on daily life
PTSD can severely impact a person’s daily life, affecting their ability to work, maintain relationships, and perform daily activities. It might lead to social isolation, difficulties in emotional regulation, and increased risk of other mental health disorders, such as depression and anxiety.
Complex PTSD
Beyond Standard PTSD
Complex PTSD (C-PTSD) is a more severe form of PTSD that develops in response to prolonged, repeated exposure to traumatic events, often where escape is not possible. C-PTSD is recognized for the depth and endurance of its impact on the individual’s life.
Origin and recognition
The concept of C-PTSD was first recognized to describe the chronic psychological stress experienced by survivors of prolonged, repeated trauma, such as prisoners of war, victims of long-term domestic violence, or individuals who experienced chronic childhood abuse.
Differences in causation
While PTSD can develop after a single event or multiple events of a shorter duration, C-PTSD is specifically tied to prolonged trauma that continues or repeats for months or even years. This distinction is crucial for understanding the depth of impact on an individual’s psyche.
Symptoms Deep Dive
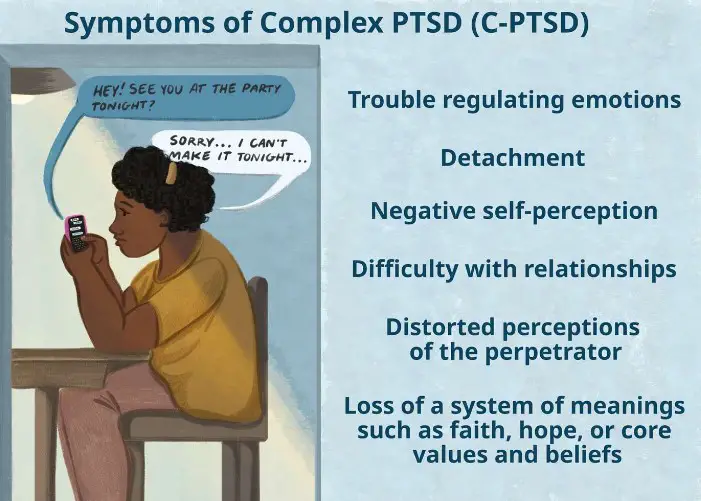
C-PTSD encompasses the symptoms of PTSD but also includes additional symptoms related to emotional regulation, self-concept, and interpersonal relationships.
Chronic nature of symptoms
Symptoms of C-PTSD are long-lasting and can be more invasive and debilitating than those of PTSD. They may include persistent sadness, suicidal thoughts, and feelings of emptiness or hopelessness.
Varied emotional responses
Individuals with C-PTSD may experience difficulty controlling emotions, leading to sudden bouts of anger, sadness, or despair. They might also have chronic feelings of guilt or shame and a persistent sense of worthlessness.
Key Differences
Duration and Exposure
One of the primary distinctions between PTSD and C-PTSD is the duration and type of trauma. PTSD typically results from a single event or a series of events over a short period, whereas C-PTSD stems from continuous, repeated trauma over months or years.
Symptoms and Complexity
Comparison of symptomatology
While both disorders share common symptoms like flashbacks and severe anxiety, C-PTSD includes additional symptoms such as difficulty with relationships, distorted perceptions of the perpetrator, and loss of faith or hope.
Recovery and Treatment
Approaches for PTSD vs. Complex PTSD
The treatment for PTSD and C-PTSD can overlap, but due to the complexity of C-PTSD, treatments often need to be more prolonged and intensive.
For PTSD, treatments may include:
- Cognitive Behavioral Therapy (CBT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Medication to manage symptoms
For Complex PTSD, treatment may also involve:
- Long-term therapy focusing on emotional regulation and interpersonal skills
- Intensive outpatient programs
- Group therapy to build support networks
Diagnosis Challenges
Overlapping Symptoms
Post-Traumatic Stress Disorder (PTSD) and Complex PTSD (C-PTSD) share many symptoms, making the diagnosis process challenging. Both disorders can present with flashbacks, anxiety, and avoidance behaviors, complicating the differentiation between them. The key to accurate diagnosis lies in understanding the duration and nature of the trauma, as well as the depth of the symptoms experienced.
Diagnostic criteria and challenges
The diagnostic criteria for PTSD, as outlined in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), focus on specific types of trauma exposure, the presence of intrusion symptoms, avoidance behaviors, negative alterations in cognition and mood, and alterations in arousal and reactivity. For C-PTSD, the criteria extend to include difficulties in emotional regulation, consciousness, self-perception, distorted perceptions of the perpetrator, relations with others, and systems of meaning.
Challenges in diagnosis arise from the subjective nature of these symptoms and the individual variability in trauma response. Moreover, symptoms of C-PTSD often overlap with other mental health disorders, such as borderline personality disorder, making it even harder to pinpoint.
Professional Insight
Importance of accurate diagnosis
An accurate diagnosis is crucial for effective treatment and recovery. It ensures that individuals receive the appropriate care tailored to their specific experiences and symptoms. Mental health professionals must consider the entire scope of an individual’s history and symptoms to differentiate between PTSD and C-PTSD accurately. This careful consideration can prevent misdiagnosis and ensure that the therapeutic approach addresses the root causes of the trauma, rather than just the surface-level symptoms.
Treatment Approaches
PTSD Treatments
Conventional therapies
For PTSD, several conventional therapies have proven effective:
- Cognitive Behavioral Therapy (CBT) helps patients understand and change the thought patterns that are disturbing their life.
- Prolonged Exposure Therapy encourages individuals to gradually approach trauma-related memories, feelings, and situations they have been avoiding.
- Eye Movement Desensitization and Reprocessing (EMDR) aims to help patients process and integrate traumatic memories.
These therapies, often combined with medication like SSRIs or SNRIs, can significantly reduce PTSD symptoms, helping individuals regain control over their lives.
Complex PTSD Strategies
Tailored interventions and support
C-PTSD requires more tailored interventions due to the complexity of the symptoms and the depth of the trauma involved. Treatment strategies may include:
- Trauma-informed care, which recognizes the widespread impact of trauma and understands paths for recovery.
- Dialectical Behavior Therapy (DBT), which focuses on improving emotional regulation and interpersonal effectiveness.
- Somatic experiencing, a body-oriented approach to help relieve the symptoms of PTSD and C-PTSD by focusing on the client’s perceived body sensations (or somatic experiences).
In addition, support groups and community resources can provide invaluable support, offering a sense of belonging and shared experience that can be therapeutic.
Living with PTSD/Complex PTSD
Personal Stories
Real-life impacts
The impact of PTSD and C-PTSD extends far beyond the individual, affecting families, relationships, and communities. Personal stories of those living with these conditions highlight the ongoing struggle with trauma but also the possibility of recovery. From veterans dealing with the aftermath of combat to survivors of abuse finding strength in their journey towards healing, these stories can inspire hope and offer insight into the resilience of the human spirit.
Coping Mechanisms
Strategies and support systems
Living with PTSD or C-PTSD requires a comprehensive approach to manage symptoms and improve quality of life. Some effective coping mechanisms include:
- Establishing a routine to provide structure and a sense of normalcy.
- Mindfulness and relaxation techniques, such as meditation or yoga, to help manage anxiety and stress.
- Physical activity, which can reduce symptoms of depression and anxiety.
- Connecting with others, whether through support groups, therapy, or with friends and family, to reduce feelings of isolation.
Building a robust support system is crucial. This can include professionals like therapists and doctors, as well as personal connections with friends and family. Online forums and support groups specifically for PTSD and C-PTSD sufferers can also provide a sense of community and understanding.
Frequently Asked Questions
What is PTSD?
PTSD, or Post-Traumatic Stress Disorder, is a mental health condition that can develop after a person has experienced or witnessed a life-threatening or traumatic event. It is characterized by intense, disturbing thoughts and feelings related to the experience that persist long after the event has ended. Individuals with PTSD may relive the event through flashbacks or nightmares; they may feel sadness, fear, or anger; and they may feel detached or estranged from other people.
How does Complex PTSD differ from PTSD?
Complex PTSD is a more severe form of PTSD that develops in response to prolonged, repeated trauma, often occurring in situations where the victim has little or no chance of escape, such as in cases of domestic violence, long-term abuse, or captivity. It encompasses a wider range of symptoms, including difficulties in emotional regulation, a persistent sense of worthlessness, and relationship challenges. These symptoms are in addition to the core symptoms of PTSD, making C-PTSD more complex to diagnose and treat.
Can children develop Complex PTSD?
Yes, children can develop Complex PTSD, especially if they are exposed to ongoing trauma, such as physical, emotional, or sexual abuse, neglect, or living in a war-torn environment. Children may exhibit symptoms differently than adults, showing signs through behavior such as aggression, difficulty in forming attachments, developmental delays, or regressive behaviors. Early intervention and supportive therapeutic environments are crucial for helping children heal from complex trauma.
Are there effective treatments for PTSD and Complex PTSD?
Effective treatments for both PTSD and Complex PTSD include psychotherapy approaches such as Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and trauma-focused therapy. Medications may also be prescribed to help manage symptoms. For Complex PTSD, treatments may also involve long-term therapy to address interpersonal relationship issues, emotional regulation, and self-concept. The key is a personalized approach that addresses the individual’s specific experiences and symptoms.
Conclusion
Understanding the distinction between PTSD and Complex PTSD is more than an academic exercise; it’s a critical step towards providing effective care and support for those affected by trauma. The nuanced differences between these conditions highlight the spectrum of trauma’s impact on the mind and underscore the need for tailored therapeutic approaches. Recognizing and treating these conditions as distinct entities allows for more accurate diagnoses, better-targeted treatments, and ultimately, more effective healing and recovery for survivors.
The journey from trauma towards recovery is deeply personal and varies widely among individuals. However, with the right support and understanding, healing is possible. Awareness and education are key in destigmatizing these conditions and in fostering environments where individuals feel safe to seek the help they need. As we continue to expand our understanding of PTSD and Complex PTSD, we open new paths to resilience, recovery, and hope for those affected by trauma.