The human reproductive system, complex and finely tuned, operates through a series of cyclical processes, notably the ovarian and menstrual cycles. These cycles play pivotal roles in fertility, hormonal balance, and overall health. Despite their interconnectedness, they harbor distinct characteristics, functions, and phases, each integral to the reproductive and endocrine systems.
The ovarian cycle refers to the series of events in the ovaries leading to the release of an egg, while the menstrual cycle describes the preparation of the uterine lining for potential pregnancy and its subsequent shedding if pregnancy does not occur. Together, these cycles constitute the monthly reproductive process in females, but they differ in their phases, hormonal changes, and physiological effects.
Understanding the nuances between the ovarian and menstrual cycles is not just an academic pursuit; it is crucial for recognizing normal bodily functions, identifying potential health issues, and managing fertility. By discerning the intricate dance between these cycles, individuals gain insights into their bodies, enabling informed health decisions and discussions with healthcare providers.
Basics of Ovarian Cycle
Definition and Role
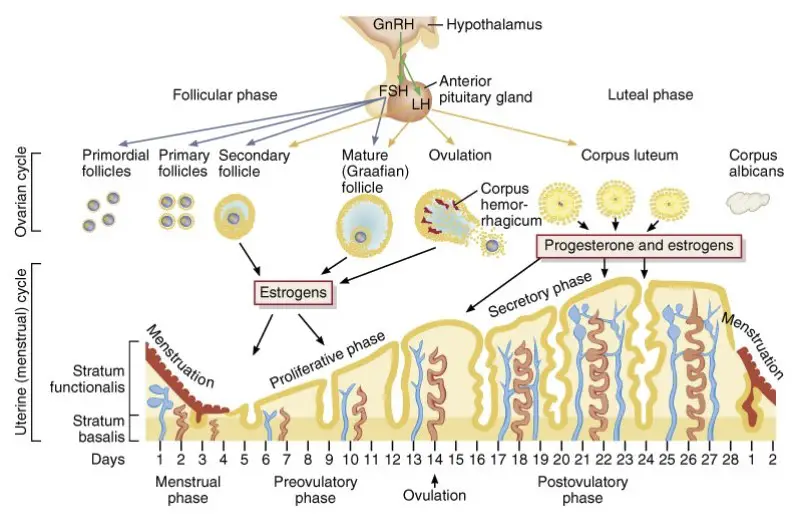
The ovarian cycle is a series of events in the ovaries that leads to the maturation and release of an egg, or ovum. This cycle is integral to reproduction, as it prepares the egg for fertilization. It’s divided into three main phases: the follicular phase, ovulation, and the luteal phase.
Phases Overview
Follicular Phase
- Starts on the first day of menstruation and ends with ovulation.
- Dominated by the growth of follicles in the ovaries under the influence of follicle-stimulating hormone (FSH).
- Estrogen levels rise, promoting the uterine lining’s growth, preparing for potential pregnancy.
Ovulation
- Marks the release of a mature egg from the ovary.
- Triggered by a surge in luteinizing hormone (LH).
- The egg then travels down the fallopian tube, where it may meet sperm and become fertilized.
Luteal Phase
- Begins after ovulation and lasts until menstruation starts.
- Characterized by the corpus luteum, which secretes progesterone.
- Progesterone prepares the uterine lining for implantation of a fertilized egg, supporting early pregnancy.
Basics of Menstrual Cycle
Definition and Purpose
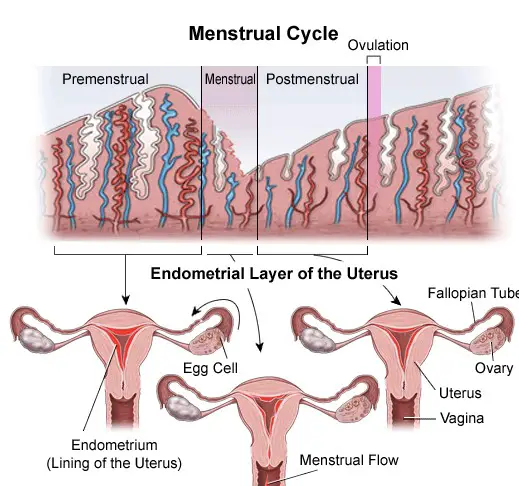
The menstrual cycle is the monthly process by which the female body prepares for potential pregnancy, with the shedding of the uterine lining if pregnancy does not occur. This cycle is marked by menstruation, the proliferative phase, and the secretory phase.
Phases Overview
Menstruation
- The shedding of the uterine lining.
- Lasts about 3 to 7 days.
- Signals the start of a new menstrual cycle.
Proliferative Phase
- Follows menstruation, lasting until ovulation.
- The uterine lining regrows, driven by rising estrogen levels.
- Prepares the uterus for a potential fertilized egg.
Secretory Phase
- Occurs after ovulation.
- The uterine lining thickens, rich in nutrients, ready to support a fertilized egg.
- If no fertilization occurs, this phase transitions back into menstruation.
Key Differences
Cycle Initiation and Duration
- The ovarian cycle initiates with follicle development in the ovaries, while the menstrual cycle begins with the shedding of the uterine lining.
- Duration can vary, with the ovarian cycle typically spanning 28 days and the menstrual cycle having similar variance.
Hormonal Changes
- The ovarian cycle’s key hormones are FSH and LH, focusing on the egg’s maturation and release.
- The menstrual cycle is dominated by estrogen and progesterone, regulating the uterine lining’s preparation and shedding.
Physiological Effects
- The ovarian cycle’s main event is ovulation, leading to the egg’s release.
- The menstrual cycle’s hallmark is menstruation, the shedding of the uterine lining.
Hormones Involved
Estrogen and Progesterone
- Estrogen is crucial for thickening the uterine lining and regulating the menstrual cycle.
- Progesterone stabilizes the uterine lining in the second half of the menstrual cycle and supports early stages of pregnancy.
Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH)
- LH is responsible for triggering ovulation and the development of the corpus luteum.
- FSH stimulates the growth of ovarian follicles, preparing an egg for ovulation.
Role and Impact on Each Cycle
- These hormones not only dictate the timing and progression of the ovarian and menstrual cycles but also influence overall reproductive health. Their balanced interplay is essential for the successful maturation of an egg, its release, and the preparation of the uterus for pregnancy.
Physical Signs and Symptoms
Understanding the physical signs and symptoms associated with the ovarian and menstrual cycles can provide critical insights into a woman’s reproductive health. These indicators can vary widely among individuals but serve as essential clues to normal processes or potential health issues.
Ovarian Cycle Indicators
The ovarian cycle involves several physical signs that may be subtle or more pronounced, depending on the individual. Key indicators include:
- Mid-cycle pain or discomfort (often referred to as mittelschmerz) can occur around the time of ovulation, signaling the release of an egg from the ovary.
- Changes in cervical mucus become more apparent, with mucus becoming thinner, clearer, and more slippery, akin to egg whites, during ovulation, facilitating sperm movement towards the egg.
- Breast tenderness or swelling can occur during the second half of the cycle, influenced by hormonal shifts.
Menstrual Cycle Indicators
The menstrual cycle presents more noticeable signs and symptoms, including:
- Menstrual bleeding, the most evident sign, marks the beginning of the cycle.
- Pre-menstrual syndrome (PMS) symptoms, such as mood swings, bloating, and cravings, occur in the days leading up to menstruation.
- Changes in basal body temperature can be monitored, with a slight decrease just before ovulation and an increase following ovulation.
Fertility Implications
Understanding fertility implications requires knowledge of the ovulation and conception window within the ovarian and menstrual cycles. This understanding is crucial for planning or preventing pregnancy.
Ovulation and Conception Window
- Ovulation marks the fertile window when an egg is released and can be fertilized by sperm. This typically occurs mid-cycle, about 14 days before the start of the next menstrual period.
- The conception window is relatively short, as the egg remains viable for about 12 to 24 hours after release. However, sperm can live in the female reproductive tract for up to 5 days, extending the fertile window to about 5-6 days.
Menstrual Health and Fertility
- Regular menstrual cycles are often a sign of good reproductive health and fertility. Irregular or absent cycles can indicate potential fertility issues or other health problems.
- Monitoring menstrual health, including cycle length, symptoms, and regularity, can provide valuable information for fertility planning and health assessment.
Health Issues Related
Several health issues are related to the ovarian and menstrual cycles, affecting a significant number of women at some point in their lives.
Common Disorders Associated with Each Cycle
- Polycystic Ovary Syndrome (PCOS) affects the ovarian cycle by causing irregular ovulation or absence of ovulation, leading to irregular menstrual cycles.
- Endometriosis involves the growth of uterine tissue outside the uterus, affecting both the menstrual and ovarian cycles by causing severe pain, irregular bleeding, and potentially infertility.
- Menstrual disorders, such as dysmenorrhea (painful periods), menorrhagia (heavy menstrual bleeding), and amenorrhea (absence of menstruation), impact the menstrual cycle.
Impact on Women’s Health
- These disorders can significantly impact a woman’s quality of life, fertility, and overall health. Early detection and management are crucial for preventing long-term complications.
Management and Care
Effective management and care strategies are essential for maintaining reproductive health and addressing any issues related to the ovarian and menstrual cycles.
Tracking and Monitoring
- Tracking cycles using apps or calendars can help women identify irregularities, understand their fertility window, and monitor for signs of potential health issues.
- Basal body temperature and cervical mucus changes can be tracked to identify ovulation and fertile windows for those planning or preventing pregnancy.
Lifestyle and Dietary Influences
- Dietary choices, such as consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, can support hormonal balance and reproductive health.
- Regular exercise and maintaining a healthy weight are beneficial for managing symptoms and reducing the risk of disorders like PCOS.
Medical Interventions
- Hormonal therapies, such as birth control pills, can regulate menstrual cycles, reduce symptoms of disorders like PCOS and endometriosis, and aid in fertility management.
- Surgery may be necessary in severe cases of disorders like endometriosis to remove excess tissue and relieve pain or fertility issues.
Frequently Asked Questions
What triggers the start of the ovarian and menstrual cycles?
The start of both cycles is triggered by hormonal signals from the brain to the ovaries. The follicle-stimulating hormone (FSH) initiates the ovarian cycle, encouraging the growth of ovarian follicles. The menstrual cycle begins with the shedding of the uterine lining, marking the first day of menstruation.
How do hormonal changes affect these cycles?
Hormonal changes are central to both the ovarian and menstrual cycles. In the ovarian cycle, estrogen and progesterone levels rise and fall, guiding the egg’s maturation and release. For the menstrual cycle, these hormones prepare the uterine lining for pregnancy and cause it to shed if pregnancy does not occur, leading to menstruation.
Can the ovarian and menstrual cycles indicate health issues?
Yes, irregularities in the ovarian and menstrual cycles, such as absent periods, excessively painful menstruation, or irregular ovulation, can indicate underlying health issues. Conditions like polycystic ovary syndrome (PCOS), endometriosis, and hormonal imbalances may manifest through disruptions in these cycles.
How can one track these cycles?
Tracking these cycles can be done using various methods, including calendar tracking, monitoring basal body temperature, and observing cervical mucus changes. Mobile apps and health trackers offer digital solutions for tracking these cycles, providing insights into fertility windows and menstrual health.
Conclusion
The distinction between the ovarian and menstrual cycles is fundamental to understanding female reproductive health. These cycles, with their unique phases and hormonal orchestration, not only facilitate reproduction but also reflect an individual’s overall well-being. Acknowledging their differences empowers individuals to monitor their health, recognize signs of potential issues, and seek appropriate care.
In fostering awareness and knowledge of these cycles, we support a broader dialogue on women’s health, encouraging proactive health management and demystifying aspects of female biology. This understanding is a stepping stone to enhanced health, well-being, and fertility management for individuals worldwide.

