Antigens are crucial biomolecules in the complex world of immunology, playing pivotal roles in health and disease. They are substances that can induce an immune response in the body, leading to the production of antibodies. This interaction is fundamental to both adaptive immunity and numerous medical diagnostics.
The O and H antigens are specific types of substances found on the surface of red blood cells that differ significantly in their structure and function. The O antigen, a part of the ABO blood group system, is characterized by its absence, giving the O blood group its universal donor status. In contrast, the H antigen serves as a foundational structure for the A and B antigens and is present in all blood groups, affecting compatibility and immune reactions during blood transfusions.
These antigens are not only critical in transfusion medicine but also play significant roles in the pathogenesis of various diseases and are targets for therapeutic interventions. Their understanding aids in better management of transfusions, understanding compatibility in organ transplantation, and developing diagnostic techniques.
Antigen Basics
Definition and Role
Antigens are molecular structures that trigger the immune system to produce an immune response. These are typically proteins or polysaccharides found on the surface of pathogens like viruses, bacteria, or on cells and tissues, including those transplanted from one individual to another. The primary role of antigens is to be recognized by the immune system, which leads to the production of antibodies, a critical component in fighting infections and in vaccine efficacy.
Types of Antigens
There are several types of antigens, each with unique features and roles:
- Exogenous antigens: These come from outside the body, typically from bacteria, viruses, or fungi. They enter the body through inhalation, ingestion, or skin penetration.
- Endogenous antigens: These are generated within cells as a result of normal cell metabolism or due to infection by a virus. They are presented on the cell surface by MHC class I molecules.
- Autoantigens: These are components of normal cells and tissues but may be recognized as foreign if the immune system becomes dysfunctional, leading to autoimmune diseases.
- Neoantigens: These are associated with tumor cells and are not present in normal cells. They can be targets for cancer immunotherapy.
O Antigen Overview
Structure Characteristics
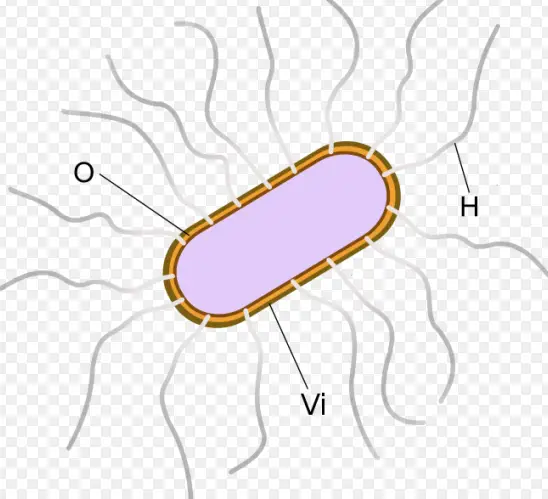
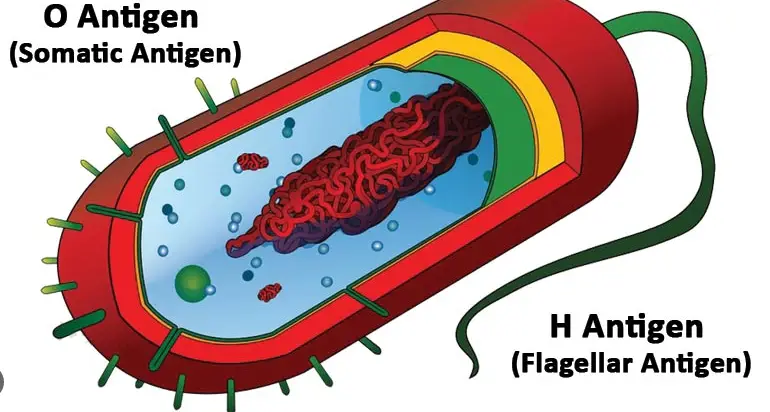
The O antigen is part of the lipopolysaccharide layer found on the outer membrane of Gram-negative bacteria. It is composed of sugar molecules and varies significantly between different bacterial species. This variation is a primary reason for the diversity of immune responses to different bacterial infections.
Biological Function
The O antigen serves several biological functions:
- Protects bacteria from the host’s immune system by impeding the effective action of phagocytes and complement system components that would otherwise attack the bacterial cell.
- Modulates the immune response: By varying its structure, the O antigen can influence the type and effectiveness of the immune response elicited.
- Role in virulence: Certain pathogenic bacteria can enhance their infectivity and survival within a host through the structural modifications of their O antigen.
H Antigen Explained
Composition Details
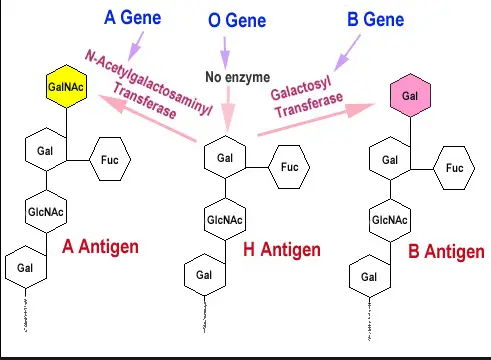
The H antigen, located on the surface of red blood cells, is a glycoprotein that forms the foundation for the A and B antigens in the ABO blood group system. In individuals with O blood type, the H antigen remains unmodified, whereas, in A and B types, it is modified by specific enzymes that add sugars to its structure.
Functional Significance
The H antigen’s primary function is its role in the ABO blood group system and compatibility in blood transfusions. It is the precursor for A and B antigens and determines an individual’s blood type:
- Blood type O: Only H antigens are present, making the blood potentially a universal donor type.
- Blood type A: The H antigen is modified to form A antigen.
- Blood type B: The H antigen is modified to form B antigen.
Comparison Factors
Structural Distinctions
The O and H antigens differ significantly in their molecular structure:
- O Antigen: Composed of repeating oligosaccharide units, which can vary between bacteria leading to the extensive antigenic diversity seen in pathogens like E. coli.
- H Antigen: Consists of a fundamental structure that can be altered by specific enzymes to form either the A or B antigen, making it relatively consistent across different individuals, except for those with certain genetic mutations.
Functional Differences
The functional implications of these structural distinctions are substantial:
- Immune response modulation: The O antigen’s variability helps bacteria evade the host’s immune system, whereas the H antigen’s consistency helps maintain blood type stability across populations.
- Role in transfusion and transplantation: Understanding these differences is crucial for safe blood transfusions and organ transplants, as mismatches in these antigens can lead to severe immune reactions.
Interaction with Immune System
O Antigen Immune Response
The immune response to the O antigen is a pivotal aspect of how our bodies defend against bacterial infections. When a pathogen with O antigens invades the body, the immune system recognizes these antigens as foreign and mounts a response. Here’s what happens:
- Antibody production: The immune system produces specific antibodies that bind to the O antigen, effectively marking the invading cells for destruction.
- Phagocytosis enhancement: Once antibodies are bound to antigens, phagocytes are more effective at engulfing and destroying the bacterial cells.
- Complement system activation: Antibody-antigen binding also activates the complement system, which helps in killing bacteria, signaling other immune cells, and clearing debris.
This immune response is crucial in controlling infections caused by bacteria that present O antigens and can be the basis for vaccine development, where components of the O antigen are used to elicit an immune response without causing disease.
H Antigen Immune Response
The response to the H antigen is more complex due to its involvement in the blood type system. Unlike the O antigen, the H antigen is naturally occurring in all humans but can still trigger an immune response if perceived as foreign, such as during a blood transfusion. Here’s the process:
- Blood type compatibility: If blood with incompatible H antigens (in terms of ABO blood types) is transfused, the recipient’s immune system can attack the donor red blood cells, seeing them as foreign.
- Antibody response: People produce natural antibodies against A and B antigens that they do not possess. Since the H antigen is the precursor to these, its modifications determine whether these antibodies will react.
Clinical Relevance
Importance in Transfusions
Understanding the role of O and H antigens in blood transfusions is critical for preventing adverse reactions and ensuring patient safety. Here’s why these antigens are vital:
- Universal donors and recipients: People with O negative blood are often called universal donors because their red blood cells can be transfused to almost any patient without concern for ABO compatibility. This is due to the lack of A, B, and Rh antigens.
- Transfusion reactions prevention: Proper matching of blood types, based on the presence or absence of these antigens, prevents potentially fatal transfusion reactions.
Role in Disease Diagnosis
Both O and H antigens play roles in the diagnosis of various diseases. For instance:
- Pathogen identification: The presence of specific O antigens can help identify bacterial strains, crucial for diagnosing infections and determining treatment strategies.
- Autoimmune disorders: Abnormal responses to H antigens can indicate autoimmune conditions where the body mistakenly attacks its own cells.
Research and Innovations
Recent Studies on O and H Antigens
Recent research has shed light on the nuanced roles of O and H antigens, with studies highlighting:
- Vaccine development: New vaccines targeting specific O antigens are in development, aiming to offer protection against a broader range of bacterial strains.
- Genetic studies: Advances in genetic profiling of the H antigen have improved our understanding of rare blood types and their implications in transfusion medicine.
Future Implications in Healthcare
The ongoing research into O and H antigens holds promising implications for healthcare:
- Improved transfusion protocols: Enhanced understanding of antigenic profiles may lead to more refined and safer transfusion practices.
- Targeted therapies: With better comprehension of antigenic differences, more effective and personalized therapies can be developed, particularly for conditions like autoimmune diseases and allergies where immune system modulation plays a crucial role.
Frequently Asked Questions
What are antigens?
Antigens are molecules capable of stimulating an immune response. They are typically foreign substances from pathogens like bacteria and viruses, but can also include other substances like chemicals, drugs, or allergens.
How do O and H antigens differ?
The O antigen differs from the H antigen primarily in its genetic expression. The O blood type lacks antigens on its red blood cells, making it a universal donor, while the H antigen acts as a precursor to the A and B antigens found in other blood types.
Why are O and H antigens important?
The O and H antigens are vital for blood transfusions and organ transplant compatibility. They help determine a person’s blood type and can affect the immune system’s reaction to transfused blood or transplanted organs.
What role do O and H antigens play in disease?
O and H antigens influence the susceptibility and severity of certain infectious diseases. They also impact the effectiveness of vaccines and the development of auto-immune disorders.
Conclusion
The differentiation between O and H antigens represents a fundamental aspect of immunology that impacts various medical fields. Their study not only enhances our understanding of immune responses but also improves clinical practices related to blood transfusion and organ transplantation.
Understanding these antigens enables healthcare professionals to manage patient care more effectively, ensuring better outcomes in treatments involving blood products and organ transplants. This knowledge continues to guide research in immunology, paving the way for innovative treatments and diagnostics in medical science.