Corneal diseases affect millions worldwide, leading to diminished vision or blindness if left untreated. Among the therapeutic strategies developed, corneal transplantation has emerged as a beacon of hope for those suffering from severe ocular surface disorders. Two advanced techniques, keratolimbal allograft (KLAL) and autologous limbal stem cell graft (ALSCG), have been at the forefront, offering new possibilities for recovery and vision restoration.
The key difference between KLAL and ALSCG lies in the source of the transplant material. KLAL involves the transplantation of limbal stem cells from a donor to the recipient’s eye, while ALSCG utilizes the patient’s own healthy tissue for the procedure. This distinction not only influences the surgical approach and potential for rejection but also significantly impacts the outcome and recovery process for patients.
These procedures are pivotal for patients with conditions leading to limbal stem cell deficiency, a critical component in corneal health and regeneration. By replenishing the limbal stem cell population, both KLAL and ALSCG aim to restore the cornea’s integrity, offering a path towards improved vision and quality of life for those affected by debilitating corneal conditions.
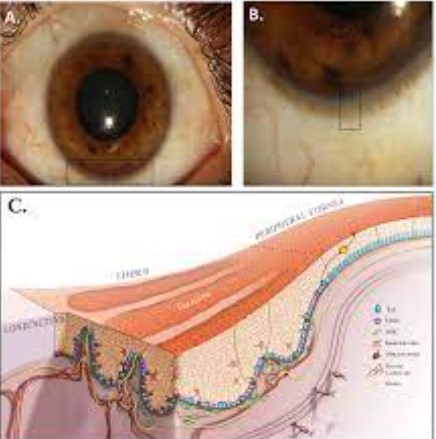
Eye Anatomy and Limbal Stem Cells
Cornea’s Role
The cornea is the eye’s front window, vital for vision. It acts as a barrier against dirt, germs, and other harmful particles. The cornea also plays a crucial role in focusing light onto the retina, allowing us to see clearly. Without a healthy cornea, our vision becomes blurred, or in severe cases, we may lose sight entirely.
Limbal Stem Cells
Just adjacent to the cornea is a critical area known as the limbus. This area houses limbal stem cells (LSCs), essential for the regeneration and healing of the corneal surface. These cells replenish the cornea’s outermost layer, keeping our vision clear and our eyes healthy. A loss or dysfunction of these cells leads to a condition called limbal stem cell deficiency (LSCD), which can significantly impair vision.
Importance in Corneal Health
Limbal stem cells are the guardians of corneal clarity and health. They repair the cornea from daily wear and tear and injuries. Without these cells, the cornea would become opaque, leading to vision loss. Maintaining a healthy population of limbal stem cells is crucial for sustaining vision and eye health.
Corneal Transplantation Overview
Indications for Surgery
Corneal transplantation becomes necessary when the cornea is damaged beyond repair due to injury, disease, or congenital defects. Conditions such as keratoconus, corneal ulcers, and scarring from infections or injuries can lead to significant vision loss, requiring transplantation.
Conditions Requiring Transplantation
The need for transplantation arises in cases of severe corneal opacity, scarring, or when non-surgical treatments fail to restore corneal function. Diseases like Fuchs’ dystrophy and bullous keratopathy also necessitate corneal transplantation to regain lost vision.
Transplant Techniques
Several corneal transplant techniques are available, each suited to different types of corneal conditions. These include:
- Penetrating Keratoplasty (PK): Replacement of the entire cornea.
- Lamellar Keratoplasty: Partial-thickness grafts, either anterior or posterior.
- Endothelial Keratoplasty (EK): Replacement of the cornea’s inner layer.
- Limbal Stem Cell Transplantation: Restores the limbus, including KLAL and ALSCG.
Keratolimbal Allograft (KLAL)
Definition and Purpose
Keratolimbal Allograft (KLAL) is a surgical method to treat patients with limbal stem cell deficiency. This procedure involves transplanting limbal stem cells from a donor to the recipient’s eye to regenerate the cornea’s surface.
What is KLAL?
KLAL is a life-changing surgery for individuals lacking healthy limbal stem cells, often due to chemical burns or genetic conditions.
When is it used?
KLAL is recommended for patients with bilateral LSCD, where both eyes lack healthy limbal cells and cannot supply tissue for autografting.
Procedure
The steps involved in KLAL include:
- Donor tissue preparation: Limbal tissue is harvested from a cadaveric donor.
- Recipient eye preparation: Damaged tissue is removed from the recipient’s eye.
- Transplantation: Donor limbal cells are transplanted onto the recipient’s eye.
- Post-operative care: Close monitoring and use of immunosuppressive medications to prevent rejection.
Advantages
Benefits of KLAL include the restoration of corneal surface, improved vision, and a reduced risk of infection and further damage.
Risks and Complications
Potential drawbacks involve rejection of the donor tissue, infections, and the need for long-term immunosuppression.
Autologous Limbal Stem Cell Graft (ALSCG)
Definition and Purpose
Autologous Limbal Stem Cell Graft (ALSCG) involves using the patient’s own tissue, typically from the other, healthy eye, to repair the damaged cornea.
What is ALSCG?
ALSCG is a procedure designed for patients with unilateral LSCD, offering a personalized approach to corneal regeneration.
Ideal Scenarios for Use
ALSCG is best suited for patients with one healthy eye capable of donating tissue, minimizing the risk of rejection.
Procedure
The key steps in ALSCG include:
- Tissue harvesting: Limbal cells are collected from the healthy eye.
- Recipient eye preparation: The eye is prepared to receive the graft.
- Transplantation: The harvested cells are transplanted to the affected eye.
- Recovery: Post-operative care focuses on healing and monitoring for complications.
Advantages
ALSCG offers high success rates, a lower risk of rejection, and eliminates the need for donor tissue.
Risks and Complications
Challenges include potential damage to the donor site and the risk of developing LSCD in the healthy eye.
KLAL vs. ALSCG
Suitability
Choosing between KLAL and ALSCG hinges on the patient’s condition and availability of healthy limbal cells. KLAL is ideal for individuals with bilateral limbal stem cell deficiency where no healthy eye tissue is available for donation. This method requires sourcing cells from a donor, increasing the complexity of post-operative care due to the risk of rejection. On the other hand, ALSCG is suitable for patients with unilateral limbal stem cell deficiency, allowing them to use their own cells for the transplantation, significantly reducing the risk of rejection and the need for immunosuppressive therapy.
Success Rates
Success rates for both KLAL and ALSCG can vary widely, influenced by factors such as the underlying cause of limbal stem cell deficiency, the patient’s overall health, and the care received both during and after the procedure. Generally, ALSCG boasts higher success rates due to the use of the patient’s own tissue, minimizing the body’s immune response. However, KLAL remains a critical option for those without the possibility of an autologous graft, offering a chance for vision restoration albeit with a higher risk of complications.
Recovery and Rehabilitation
Post-surgery, patients can expect a recovery period that involves close monitoring, medication to promote healing and prevent rejection, and possibly additional surgeries to achieve optimal results. KLAL patients often require a longer course of immunosuppressive drugs to prevent graft rejection. ALSCG recipients may have a shorter recovery period due to the lower risk of rejection but must also protect the donor site to prevent limbal stem cell deficiency in the healthy eye.
- Eye protection: Patients must safeguard their eyes from physical trauma and excessive light.
- Medication regimen: Adherence to prescribed medications is critical for preventing infection and rejection.
- Follow-up appointments: Regular check-ups allow for timely interventions if complications arise.
Cost Considerations
The cost of KLAL and ALSCG procedures can vary significantly, influenced by factors such as the surgical setting, the need for donor tissue, and the length of post-operative care. ALSCG may be less costly in the long run due to shorter recovery times and less need for expensive immunosuppressive medications. However, the financial aspect should be weighed against the clinical outcomes and the patient’s specific condition.
Patient Selection Criteria
The decision to proceed with KLAL or ALSCG depends on several key factors:
- Extent of limbal stem cell deficiency: Is the condition unilateral or bilateral?
- Availability of healthy tissue: Does the patient have a healthy eye that can donate tissue?
- Overall health and immune system status: Can the patient tolerate immunosuppressive therapy if needed?
- Patient’s lifestyle and compliance: Will the patient be able to follow the post-operative care regimen?
Future Directions
Advances in Corneal Transplantation
The field of corneal transplantation is rapidly evolving, with ongoing research focused on improving outcomes and reducing risks associated with these life-changing procedures. Innovations such as lab-grown limbal stem cells and gene therapy offer promising avenues for treating limbal stem cell deficiency more effectively and with fewer complications.
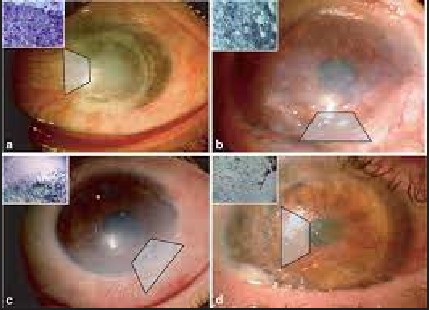
Emerging Technologies and Methods
Technological advancements are paving the way for less invasive and more successful corneal transplants. Techniques like in vivo confocal microscopy allow for precise assessment of limbal stem cell function, improving patient selection and treatment planning. Furthermore, the development of bioengineered corneas holds the potential to overcome the limitations of traditional donor tissue, offering a renewable source of material for transplantation.
Research and Trials
Current research efforts include clinical trials on stem cell therapy, tissue engineering, and the use of biomaterials to support limbal stem cell growth and integration. These studies aim not only to refine existing procedures but also to discover entirely new treatments for corneal diseases.
Frequently Asked Questions
What are limbal stem cells?
Limbal stem cells are crucial for maintaining the health and clarity of the cornea, the eye’s outermost layer. Located at the cornea’s periphery, these cells are responsible for continually regenerating the corneal epithelium, ensuring its transparency and vision functionality. Damage or deficiency in these cells can lead to serious ocular surface disorders, underscoring the importance of treatments like KLAL and ALSCG.
How do KLAL and ALSCG differ in terms of donor tissue?
The primary difference between KLAL and ALSCG lies in the origin of the transplant material. In KLAL, the limbal stem cells are sourced from a donor, either living or deceased. In contrast, ALSCG utilizes the patient’s own tissue, typically harvested from the unaffected eye. This distinction is critical in determining the procedure’s suitability, risk of rejection, and overall success.
Who is a candidate for KLAL or ALSCG?
Candidates for KLAL or ALSCG are individuals suffering from limbal stem cell deficiency due to conditions like chemical burns, Stevens-Johnson syndrome, or other ocular surface diseases. The choice between KLAL and ALSCG depends on the extent of the damage and whether healthy limbal tissue is present in either eye, guiding the personalized treatment plan.
What is the success rate of these procedures?
Success rates for KLAL and ALSCG vary based on several factors, including the underlying cause of limbal stem cell deficiency, the extent of ocular surface damage, and post-operative care. Generally, success is higher in ALSCG when viable tissue from the patient is available, reducing the risk of rejection. However, with proper selection and management, both procedures offer significant potential for visual restoration.
Conclusion
Keratolimbal allograft and autologous limbal stem cell graft represent significant advancements in treating corneal diseases, providing hope for patients with severe ocular surface disorders. By understanding the differences, advantages, and potential risks associated with each procedure, patients and clinicians can make informed decisions tailored to individual needs and conditions.
The journey towards visual restoration through corneal transplantation is complex and requires careful consideration of various factors, including the source of donor tissue, the patient’s specific condition, and the anticipated recovery process. With ongoing research and development, the future holds promise for even more effective treatments, enhancing the quality of life for those affected by corneal diseases.

