Interferons are proteins that play a crucial role in the defense mechanisms of the human body, especially when it comes to fighting off viruses and other pathogens. Among the various types of interferons, Beta interferons stand out for their significant impact on managing autoimmune diseases, including multiple sclerosis (MS). These proteins, produced through biotechnological methods, have transformed the treatment landscape for patients suffering from such conditions.
The difference between Interferon Beta 1A and Interferon Beta 1B lies primarily in their molecular structure, production process, and clinical applications. Interferon Beta 1A is derived from mammalian cells and is used in its natural form, while Interferon Beta 1B is produced in modified E. coli bacteria and is a slightly altered version of the naturally occurring protein. Both are FDA-approved for the treatment of multiple sclerosis but differ in their administration schedules, side effects, and some aspects of efficacy.
Interferon Beta 1A and 1B have provided new hope to individuals diagnosed with relapsing forms of multiple sclerosis by reducing the frequency and severity of flare-ups. Furthermore, they offer a protective effect against the formation of new lesions in the brain, as seen on MRI scans, thus slowing the progression of the disease. Their introduction has been a milestone in MS treatment, offering patients improved quality of life and better disease management options.
Interferons Explained
Overview
Interferons are a group of signaling proteins made and released by host cells in response to the presence of pathogens, such as viruses, bacteria, parasites, and also tumor cells. They are named for their ability to “interfere” with viral replication within host cells. Essentially, interferons signal the immune system to activate, protect cells from virus infections, and increase the antigen presentation so the immune system can recognize the pathogen.
Types of Interferons
There are three main types of interferons, classified based on the type of receptor through which they signal:
- Type I interferons include Interferon-alpha (IFN-α) and Interferon-beta (IFN-β), among others. They are widely known for their role in antiviral resistance.
- Type II interferon is Interferon-gamma (IFN-γ), primarily involved in the immune response to bacteria and for activating macrophages.
- Type III interferons include Interferon-lambda (IFN-λ), newer members of the interferon family with similar antiviral properties to Type I but with a more limited range of activity.
Beta Interferons
Specific Function
Interferon Beta (IFN-β) is a Type I interferon with a crucial role in managing autoimmune diseases, especially multiple sclerosis (MS). It modulates the body’s immune response to slow the progression of the disease. IFN-β reduces inflammation and the autoimmune response, protecting against the myelin sheath damage seen in MS patients.
Use in Diseases
The primary use of IFN-β is in the treatment of multiple sclerosis. It can reduce the number and severity of relapses, slow the progression of physical disability, and decrease the number of new lesions as observed in MRI scans.
Interferon Beta 1A
Overview
Definition
Interferon Beta 1A (IFN Beta 1A) is a form of beta interferon that is identical to the human protein produced in the body. It’s used as a therapeutic agent in the treatment of multiple sclerosis.
Production Method
IFN Beta 1A is produced through recombinant DNA technology in mammalian cells, usually Chinese Hamster Ovary (CHO) cells. This method allows for the production of a protein that is nearly identical to the naturally occurring interferon beta in humans.
Clinical Uses
Approved Conditions
The FDA has approved IFN Beta 1A for the treatment of patients with relapsing forms of multiple sclerosis. It helps reduce the frequency of clinical exacerbations and slows the accumulation of physical disability.
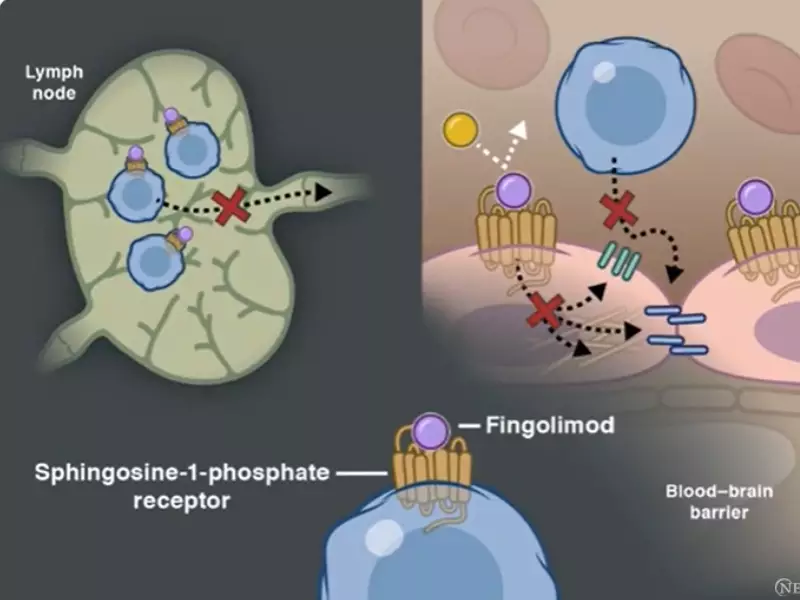
Mechanism of Action
IFN Beta 1A works by modulating the immune system, reducing inflammation that leads to demyelination in MS. It increases the production of anti-inflammatory agents while reducing pro-inflammatory cytokines, helping to protect the nervous system.
Benefits and Efficacy
Study Findings
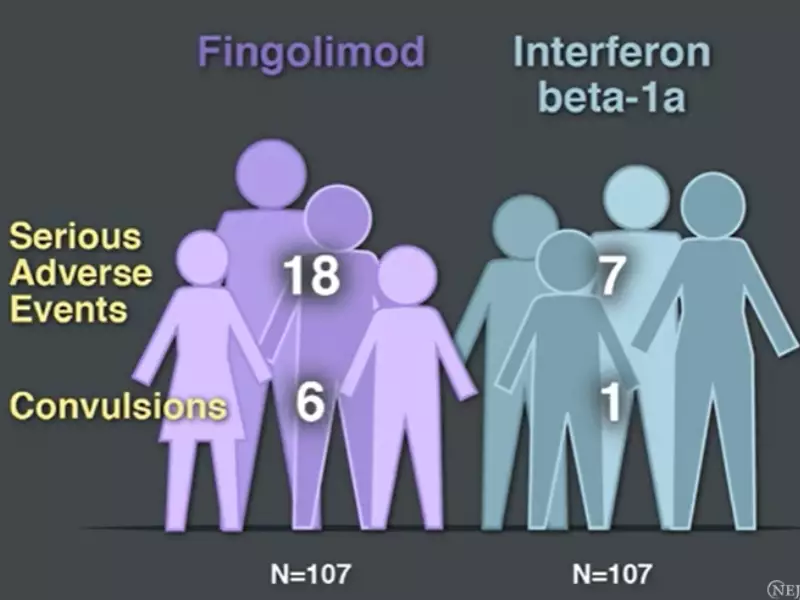
Studies have shown that IFN Beta 1A significantly reduces the rate of MS relapses and delays the progression of disability. It also leads to a reduction in new or enlarging brain lesions as seen on MRI.
Comparison with Other Treatments
Compared to other MS treatments, IFN Beta 1A offers a balance between efficacy and side effects, making it a preferred option for many patients. It’s often compared to glatiramer acetate, another first-line treatment for MS, with both showing similar efficacy but different side effect profiles.
Interferon Beta 1B
Overview
Definition
Interferon Beta 1B (IFN Beta 1B) is a modified version of the natural human protein, produced in E. coli using recombinant DNA technology. It was the first type of interferon beta approved for the treatment of MS.
Production Technique
The production of IFN Beta 1B involves the use of genetic engineering to insert the human interferon beta gene into E. coli bacteria. The bacteria then produce the interferon, which is harvested and purified for medical use.
Clinical Applications
Indications for Use
IFN Beta 1B is indicated for the treatment of relapsing-remitting multiple sclerosis. It is used to reduce the frequency of clinical exacerbations and to delay the progression of physical disability.
Action Mechanism
Like IFN Beta 1A, IFN Beta 1B modulates the immune system to reduce inflammation and autoimmunity. It alters the expression of surface antigens and increases the production of anti-inflammatory molecules, slowing the progression of MS.
Advantages and Effectiveness
Research Outcomes
Clinical trials and research studies have demonstrated that IFN Beta 1B effectively reduces the number of MS relapses and delays the accumulation of disability over time. It also shows a decrease in the formation of new lesions on MRI scans.
Stand against Alternatives
When compared to other MS therapies, IFN Beta 1B offers a unique administration schedule (every other day) and a proven track record in reducing MS relapses. Its side effect profile and effectiveness make it a competitive option, particularly for patients who may not respond well to other treatments.
Comparative Analysis
Structural Differences
Molecular Structure
The molecular structure of Interferon Beta 1A closely mimics that of the naturally occurring interferon beta in humans, as it is produced in mammalian cells. This similarity ensures that the body recognizes and uses it effectively, mirroring the action of endogenous interferons. In contrast, Interferon Beta 1B undergoes modifications during its production in E. coli bacteria. It lacks a carbohydrate side chain present in the natural and 1A forms, which leads to a slightly different biological activity.
Biological Activity
Despite these structural differences, both Interferon Beta 1A and 1B activate the same receptor pathways to exert their therapeutic effects. However, the absence of the carbohydrate side chain in Interferon Beta 1B may affect its stability and how the body metabolizes it, potentially leading to variations in efficacy and side effects.
Side Effects and Tolerability
Common Side Effects
Both interferons share common side effects, including flu-like symptoms (fever, chills, fatigue, muscle aches), injection site reactions, and potential blood abnormalities. However, due to their structural differences, patients may experience these side effects with varying degrees of severity.
Managing Side Effects
Managing the side effects of Interferon Beta 1A and 1B involves:
- Taking over-the-counter pain relievers and fever reducers
- Rotating injection sites to reduce skin reactions
- Staying hydrated and resting to alleviate flu-like symptoms
Healthcare providers may also adjust the dosage or schedule to improve tolerability.
Cost and Accessibility
Pricing Comparison
The cost of Interferon Beta 1A and 1B can vary widely based on geographical location, insurance coverage, and dosage requirements. Generally, pricing differences may arise due to the different production methods and the companies manufacturing them.
Availability in Markets
Both medications are widely available in most markets, including North America, Europe, and parts of Asia. However, accessibility can be impacted by insurance coverage, healthcare systems, and national drug policies, making some options more accessible to patients than others.
Decision Factors
Choosing Between 1A and 1B
When deciding between Interferon Beta 1A and 1B, factors to consider include:
- Efficacy in managing specific symptoms and progression of MS
- Side effect profile and patient tolerance
- Administration schedule and method
- Patient’s lifestyle and preferences
Patient-specific Considerations
Every patient’s experience with MS is unique, making individual factors crucial in treatment decisions. These include:
- Disease severity and progression
- Previous treatment responses
- Overall health and presence of other conditions
- Personal preferences and lifestyle factors
Expert Recommendations
Guidelines and Consensus
Medical societies and expert panels provide guidelines based on clinical evidence to help physicians choose between Interferon Beta 1A and 1B. These guidelines consider the overall benefit-risk profile of each medication, recommending them based on disease characteristics and patient factors.
Future Directions
Ongoing Research
Novel Formulations
Research is focused on developing new formulations of interferons that could offer better efficacy, reduced side effects, or more convenient administration schedules. These efforts aim to enhance patient adherence and improve quality of life.
Combination Therapies
Studies are exploring the potential of combining Interferon Beta with other MS treatments to achieve synergistic effects. These combinations may offer superior outcomes by targeting multiple pathways involved in the disease process.
Emerging Alternatives
Next-generation Interferons
The development of next-generation interferons promises enhanced efficacy and reduced side effects through modifications at the molecular level. These advancements could lead to treatments that are more tailored to individual patient needs.
Gene Therapy Insights
Gene therapy represents a frontier in MS treatment, with the potential to directly modify the disease process at the genetic level. While in early stages, this approach could offer a long-term solution for managing or even curing MS.
Frequently Asked Questions
How do Interferon Beta 1A and 1B work?
Interferon Beta 1A and 1B work by modulating the immune system’s response, reducing inflammation, and inhibiting the replication of viruses within the body. They help manage multiple sclerosis by preventing the immune system from attacking the myelin sheath, a protective covering of the nerves, thus reducing the frequency and severity of episodes or flare-ups in relapsing forms of the disease.
Can Interferon Beta 1A and 1B cure Multiple Sclerosis?
No, Interferon Beta 1A and 1B cannot cure Multiple Sclerosis (MS). However, they are effective in managing the symptoms of MS and slowing down its progression. By reducing the number of relapses and delaying the accumulation of physical disabilities, these medications help maintain a better quality of life for individuals living with this chronic condition.
What are the side effects of Interferon Beta 1A and 1B?
Common side effects of Interferon Beta 1A and 1B include flu-like symptoms such as fever, chills, muscle aches, and fatigue. Injection site reactions are also common, including redness, pain, or swelling. These side effects tend to decrease over time as the body adjusts to the medication. Less common but more serious side effects can include liver damage, depression, and blood cell count abnormalities, which require regular monitoring.
How often are Interferon Beta 1A and 1B administered?
Interferon Beta 1A is typically administered either once a week via intramuscular injection or three times a week via subcutaneous injection, depending on the formulation. Interferon Beta 1B is administered every other day through subcutaneous injection. The frequency of administration can influence patient preference and adherence to treatment.
Conclusion
The development of Interferon Beta 1A and 1B has marked a significant advance in the treatment of multiple sclerosis, offering patients new hope for managing this chronic and often disabling disease. By understanding the differences between these two forms of interferon, patients and healthcare providers can make informed decisions that align with individual treatment goals and preferences.
Ultimately, while both Interferon Beta 1A and 1B provide essential options in the fight against multiple sclerosis, ongoing research and development in the field of neurology promise even more innovative solutions in the future. The journey of medical advancement continues, with the goal of improving outcomes and quality of life for those affected by this challenging condition.
