Viruses are microscopic agents of disease that have shaped human history through pandemics and targeted outbreaks. Among the myriad of viral threats, hantavirus and coronavirus stand out due to their unique transmission modes and impacts on public health. These viruses, though both highly contagious, stem from different origins and involve distinct epidemiological narratives.
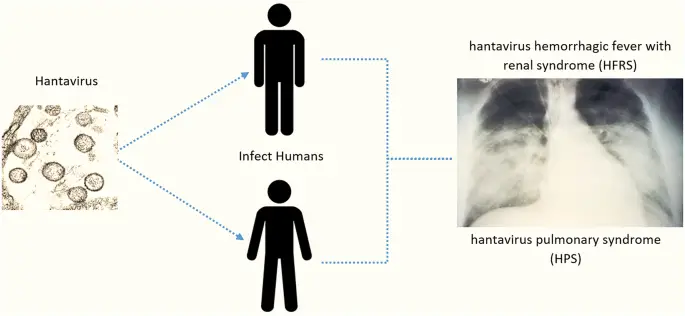
Hantavirus and coronavirus are primarily differentiated by their modes of transmission, symptoms, and the geographical areas they affect. Hantavirus is typically spread through contact with rodent carriers, primarily affecting the lungs with severe respiratory issues. In contrast, coronavirus, including its notorious SARS-CoV-2 strain responsible for COVID-19, spreads primarily through respiratory droplets, impacting both respiratory and other bodily systems.
While hantavirus outbreaks are less frequent and usually localized, coronavirus has demonstrated its ability to cause global pandemics, profoundly affecting health infrastructure and economies worldwide. Both viruses require distinct strategies for diagnosis, treatment, and prevention, highlighting the importance of tailored public health responses to manage their spread effectively.
Virus Overview
Hantavirus
Origin and Discovery
Hantavirus was first identified during the Korean War in 1951, when it led to severe illnesses among United Nations troops. However, the virus itself wasn’t isolated until 1976. The name “Hantavirus” stems from the Hantan River area in South Korea, where early outbreaks were extensively studied. These initial observations linked the virus to specific rodent species, later identified as its primary vectors.
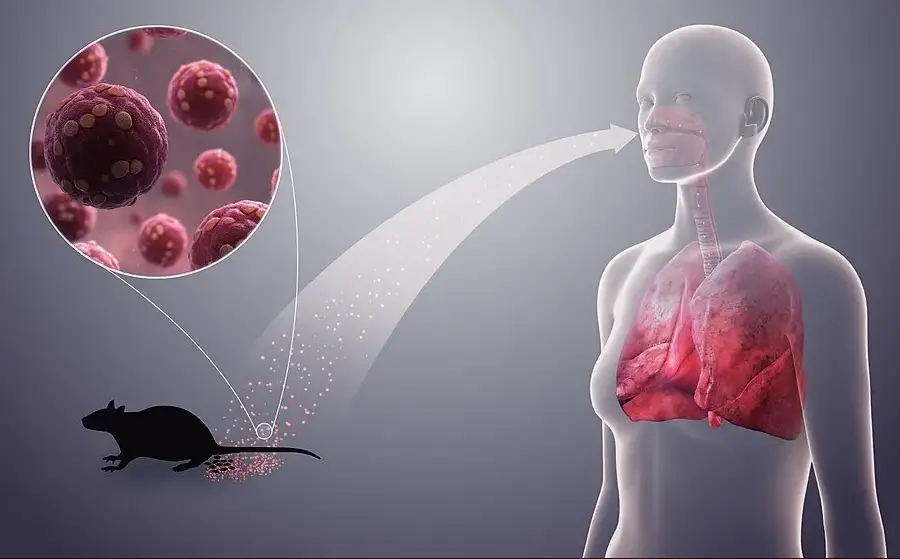
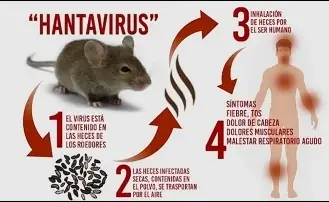
How It Spreads
Hantavirus spreads to humans primarily through airborne particles from rodent droppings, urine, or saliva that contain the virus. People can become infected by inhaling contaminated air in rodent-infested environments, such as barns, homes, or any other closed spaces where rodents have access. In rare cases, bites from infected rodents can also transmit the virus. It is crucial to note that there is no evidence of hantavirus spreading directly from person to person under normal circumstances.
Coronavirus
Origin and Discovery
The term “coronavirus” refers to a family of viruses known for causing respiratory ailments and featuring a distinctive crown-like appearance under a microscope. The common cold is a well-known illness caused by certain types of coronaviruses. However, more severe strains, like SARS-CoV (Severe Acute Respiratory Syndrome Coronavirus) and MERS-CoV (Middle East Respiratory Syndrome Coronavirus), have caused significant outbreaks in 2003 and 2012, respectively. The most recent strain, SARS-CoV-2, responsible for the COVID-19 pandemic, was first identified in Wuhan, China, in December 2019.
Modes of Transmission
Coronavirus primarily spreads through respiratory droplets when an infected person coughs, sneezes, or talks. These droplets can travel through the air and be inhaled by people nearby. Additionally, touching surfaces contaminated with the virus and then touching the face can also lead to infection. This mode of transmission highlights the importance of regular hand washing and maintaining physical distance to prevent the spread of the virus.
Symptoms Comparison
Hantavirus Symptoms
Early Signs
The early signs of Hantavirus Pulmonary Syndrome (HPS) include fatigue, fever, and muscle aches, particularly in the large muscle groups that include the thighs, hips, back, and sometimes shoulders. These symptoms are often accompanied by headaches, dizziness, chills, and abdominal problems, such as nausea, vomiting, diarrhea, and abdominal pain.
Progression and Severity
As the disease progresses, the symptoms can worsen significantly, usually within a few days, leading to severe respiratory distress. The lungs can fill with fluid, making breathing difficult and reducing the heart’s efficiency. This stage requires immediate medical attention, often involving hospitalization in intensive care units where patients may require mechanical ventilation.
Coronavirus Symptoms
Common Symptoms
The common symptoms of coronavirus infections include fever, cough, and shortness of breath. These symptoms can range from mild to severe and, in severe cases, can lead to pneumonia, acute respiratory distress syndrome, and death. Symptoms typically appear 2-14 days after exposure.
Variations by Strain
Different strains of coronavirus can lead to varying symptoms. For instance, SARS-CoV was more likely to cause severe respiratory illness, while MERS-CoV often led to rapid kidney failure. SARS-CoV-2, while it shares similarities with these strains, has shown a broader spectrum of symptoms, including loss of taste and smell, which were distinctive for the COVID-19 pandemic.
Risk Factors
Hantavirus Risks
Geographic Prevalence
Hantavirus infections have been primarily reported in rural areas of the Western United States, although cases have been documented in many countries in the Americas. The virus’s prevalence is closely associated with specific rodent populations native to these areas.
Specific Activities Increasing Risk
Activities that increase human exposure to rodent droppings can significantly raise the risk of hantavirus infection. These include:
- Cleaning rodent-infested spaces without proper safety measures.
- Living in or visiting rural and semi-rural areas where rodent populations are high.
- Engaging in outdoor activities such as camping or hiking in habitats frequented by infected rodents.
Coronavirus Risks
Global Spread Patterns
Coronavirus has demonstrated a significant ability to spread rapidly within and between countries due to its high transmission rate among humans. Factors that facilitate its spread include international travel, densely populated areas, and the virus’s ability to survive on surfaces for extended periods.
High-risk Groups
Certain populations are at higher risk for severe illness from coronavirus, including:
- Older adults, typically those aged 65 and older.
- People with underlying health conditions such as diabetes, heart disease, and lung disease.
- Individuals with weakened immune systems.
Diagnostic Methods
Detecting Hantavirus
Laboratory Tests and Criteria
Diagnosing hantavirus requires specific blood tests that can detect the viral antigens or specific antibodies produced in response to the infection. The most common tests include ELISA (enzyme-linked immunosorbent assay), which measures the antibodies, and RT-PCR (reverse transcription-polymerase chain reaction), which detects viral RNA.
Challenges in Diagnosis
The main challenges in diagnosing hantavirus stem from its similar initial symptoms to other viral infections, which can lead to misdiagnosis. Early detection is crucial, as the virus can progress rapidly to severe stages.
Detecting Coronavirus
Standard Tests Used Worldwide
The primary diagnostic tool for coronavirus is the RT-PCR test, which is highly effective in detecting the virus’s genetic material in respiratory specimens. This test is the gold standard for confirming SARS-CoV-2 infection.
Advances in Rapid Testing
Recent developments in rapid antigen testing have made it possible to detect coronavirus within minutes, providing crucial support in managing outbreaks and implementing timely quarantine measures. These tests are particularly valuable in high-throughput environments like airports or large events.
Treatment Protocols
Treating Hantavirus
Current Medical Approaches
Hantavirus treatment is primarily supportive, as there is no specific cure or vaccine available. The focus is on managing symptoms and supporting vital organ functions. Patients with severe cases of Hantavirus Pulmonary Syndrome (HPS) often require hospitalization in intensive care units where they receive treatment that may include:
- Mechanical ventilation to aid breathing.
- Oxygen therapy to maintain oxygen saturation.
- Fluid management to prevent shock and support cardiovascular function.
Prompt admission to intensive care units and supportive treatment significantly improves survival rates.
Research and Limitations
Research on hantavirus has been challenging due to its relatively rare occurrence and the severe, rapid progression of the disease. Current research focuses on understanding the virus’s pathology and developing potential antiviral treatments and vaccines. However, the sporadic nature of outbreaks and the diversity of hantavirus strains complicate these efforts.
Treating Coronavirus
Evolving Treatment Strategies
Treatment strategies for coronavirus have evolved significantly since the onset of the COVID-19 pandemic. Early treatments focused primarily on symptom management, but now include a range of approaches aimed at combating the virus and supporting the immune system. These include:
- Antiviral drugs like Remdesivir, which have been approved for treating COVID-19 in severe cases.
- Steroids such as dexamethasone, which reduce inflammation and have been shown to decrease mortality in critically ill patients.
- Monoclonal antibodies that target the virus and can prevent it from entering cells.
Role of Vaccination
Vaccination has been a critical element in managing the COVID-19 pandemic. Several vaccines have been developed at unprecedented speed, showing high efficacy in preventing severe illness and death. Ongoing vaccination efforts are crucial for achieving herd immunity and controlling the spread of the virus.
Prevention Strategies
Preventing Hantavirus
Environmental Control and Safety
To prevent hantavirus infection, controlling rodent populations and minimizing contact with them is crucial. Recommendations include:
- Sealing up homes and outbuildings to prevent rodent entry.
- Safe cleaning practices for areas contaminated by rodent droppings, including the use of disinfectants and proper ventilation.
- Rodent population control through traps and careful management of food sources that may attract rodents.
Personal Protective Measures
When cleaning areas with potential rodent infestations, wearing protective gear is essential. This includes:
- Respirators to prevent inhalation of contaminated dust.
- Gloves to avoid direct contact with contaminated materials.
- Proper disposal of rodent carcasses and waste using double-bagged plastic bags.
Preventing Coronavirus
Public Health Guidelines
Public health guidelines have been instrumental in controlling the spread of coronavirus. These guidelines include:
- Physical distancing to reduce virus transmission.
- Mask wearing in public spaces to prevent droplet spread.
- Hand hygiene practices such as regular washing and use of sanitizers.
Importance of Vaccination
Vaccination against COVID-19 is one of the most effective prevention strategies. It reduces the risk of developing severe disease, limits the spread of the virus, and contributes to community immunity.
Economic and Social Impact
Impact of Hantavirus
Case Studies of Outbreaks
Specific outbreaks of hantavirus, such as the 1993 outbreak in the Southwestern United States, highlighted the virus’s potential to cause severe health crises in localized areas. These events have had profound impacts on local economies and health services, stressing the importance of rapid response and public education.
Long-term Effects on Communities
Long-term effects of hantavirus outbreaks include increased public health surveillance and improved guidelines for dealing with rodent populations, which can have lasting impacts on community practices and local economies.
Impact of Coronavirus
Global Economic Repercussions
The global economy has been significantly affected by the COVID-19 pandemic, with impacts ranging from small businesses closing to major shifts in international trade and travel. Economic recovery is ongoing and uneven, with many countries facing deep recessions and job losses.
Changes in Social Behaviors
Social behaviors have changed dramatically due to the pandemic. These changes include increased remote working, reliance on digital communication, and adjustments in personal interactions and travel habits. These behaviors are likely to have long-lasting effects on societal norms.
Future Outlook
Research Directions
Recent Breakthroughs in Hantavirus Research
Recent advances in understanding the genetic and molecular basis of hantavirus have opened new avenues for vaccine research and potential therapies, which could pave the way for better management of future outbreaks.
Innovations in Coronavirus Management
Innovative treatments and rapid vaccine development have characterized the response to the COVID-19 pandemic. These advancements are setting new standards for dealing with viral outbreaks and highlight the importance of global cooperation in health crises.
Global Health Implications
Lessons for Future Pandemics
The experiences gained from managing hantavirus and coronavirus outbreaks provide critical lessons in pandemic preparedness, emphasizing the need for rapid response capabilities and robust public health strategies.
Importance of Viral Research
Continued viral research is essential for anticipating and mitigating future viral threats. Investing in health research and development, improving surveillance systems, and fostering international collaboration are key to better global health outcomes.
FAQs
What is Hantavirus?
Hantavirus is a zoonotic virus primarily transmitted to humans through inhalation of aerosolized particles from rodent droppings, urine, or saliva. Infection can lead to severe respiratory diseases like Hantavirus Pulmonary Syndrome (HPS), which can be fatal.
How does Coronavirus spread?
Coronavirus is predominantly spread through respiratory droplets when an infected person coughs, sneezes, or talks. It can also spread by touching surfaces contaminated with the virus, followed by touching the face, although this is not the main way the virus spreads.
What are the symptoms of Hantavirus?
Symptoms of hantavirus infection include fatigue, fever, muscle aches, especially in large muscle groups, dizziness, and chills. As the disease progresses, it can lead to severe respiratory distress and, in many cases, requires intensive care.
How is Coronavirus diagnosed?
Coronavirus is diagnosed using RT-PCR tests, which detect the virus’s genetic material in a sample taken typically from a patient’s nose or throat. Rapid antigen tests and antibody tests for previous exposure are also widely used.
Can Hantavirus cause a pandemic?
While hantavirus is dangerous, its potential for causing a pandemic is low due to its mode of transmission and the typically isolated environments of its outbreaks. Unlike respiratory viruses like coronavirus, hantavirus does not spread from person to person.
Conclusion
In reviewing hantavirus and coronavirus, it becomes clear that despite their shared classification as viruses, their impact on public health varies drastically. Hantavirus, with its specific transmission through rodents and severe respiratory effects, presents a localized threat, whereas coronavirus, capable of widespread human-to-human transmission, poses a global challenge.
The differences between these viruses underscore the need for public health strategies that are not one-size-fits-all but are instead adapted to the characteristics of specific viruses. As we move forward, the lessons learned from managing these viruses are invaluable for preparing for future viral outbreaks.