Fungal infections, a common concern for many, can range from superficial skin conditions to serious systemic diseases affecting vital organs. The development of antifungal medications like Fluconazole and Itraconazole has significantly improved the management of these infections, offering targeted treatment options. These drugs work by attacking the cell membrane of fungi, leading to their destruction and alleviating the infection.
Fluconazole and Itraconazole are both antifungal medications, but they differ in their chemical structure, spectrum of activity, absorption, metabolism, and potential drug interactions. Fluconazole is known for its effectiveness against yeast infections, such as Candida, while Itraconazole covers a broader range of fungi, including Aspergillus. Each drug has its unique advantages and specific conditions for which it is the preferred treatment.
Understanding the distinctions between Fluconazole and Itraconazole is crucial for selecting the most appropriate therapy. These differences impact not only the choice of treatment for various fungal infections but also how these medications are administered and monitored. By offering a tailored approach, healthcare professionals can maximize treatment efficacy and minimize potential risks associated with these powerful antifungal agents.
What is Fluconazole?
Overview and Usage
Fluconazole is an antifungal medication designed to combat a variety of fungal infections. It is part of a class of drugs known as triazole antifungals, which work by inhibiting the growth of fungi. Fluconazole is often prescribed for infections caused by Candida, including thrush and yeast infections in different parts of the body.
Mechanism of Action
The mechanism of action for Fluconazole involves inhibiting the enzyme lanosterol 14-α-demethylase. This enzyme is crucial for converting lanosterol to ergosterol, an essential component of the fungal cell membrane. Without ergosterol, the cell membrane cannot form properly, leading to holes and ultimately the death of the fungal cell.
Common Uses
- Oral thrush and esophageal infections: Common in individuals with weakened immune systems.
- Vaginal yeast infections: A single dose can often clear up the infection.
- Fungal skin infections: Including athlete’s foot and ringworm.
- Systemic Candida infections: Such as candidemia, a serious bloodstream infection.
Dosage and Administration
The dosage of Fluconazole varies depending on the type and severity of the infection:
- Vaginal yeast infections: Typically, a single oral dose of 150 mg.
- Other infections: May require 200 mg on the first day followed by 100 mg daily, with adjustments based on response and severity.
Always follow a healthcare provider’s instructions for dosage and duration of treatment.
What is Itraconazole?
Overview and Usage
Itraconazole is another antifungal medication, also belonging to the triazole class. It’s known for its broad spectrum of action against various fungi, making it effective for both superficial and systemic fungal infections. Itraconazole is used for conditions not typically covered by Fluconazole, including aspergillosis, blastomycosis, and histoplasmosis.
Mechanism of Action
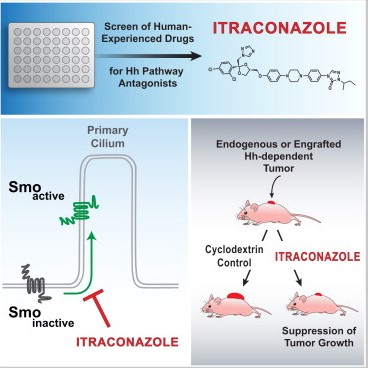
Like Fluconazole, Itraconazole works by inhibiting the enzyme responsible for ergosterol synthesis. However, its broader spectrum of activity allows it to target a wider range of fungi, making it a versatile option for treating different fungal infections.
Common Uses
- Nail fungus: Effective for both fingernail and toenail infections.
- Aspergillosis: An infection caused by the Aspergillus fungi.
- Blastomycosis and Histoplasmosis: Fungal infections affecting lungs and other organs.
- Candida infections: Especially in cases where Fluconazole is ineffective.
Dosage and Administration
Itraconazole’s dosage varies, often requiring:
- Nail fungus: 200 mg once or twice a day for 6 to 12 weeks.
- Systemic infections: Dosage may differ based on the infection type and patient response.
It’s crucial to take Itraconazole with food to enhance absorption.
Key Differences
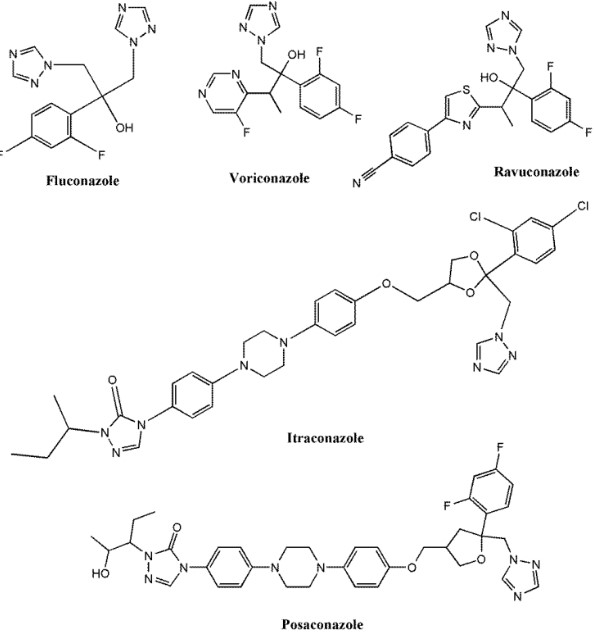
Chemical Structure
Fluconazole and Itraconazole have different chemical structures, affecting their solubility and absorption. Fluconazole is more water-soluble, which influences its administration and distribution in the body.
Spectrum of Activity
Itraconazole has a broader spectrum of activity compared to Fluconazole. It is effective against a wider variety of fungi, including those responsible for systemic infections.
Absorption and Metabolism
Fluconazole is well-absorbed orally and does not require food for its absorption. In contrast, Itraconazole needs to be taken with food to improve its bioavailability. Additionally, Fluconazole’s simpler metabolism minimizes the risk of drug interactions.
Drug Interactions
Both medications interact with other drugs, but Itraconazole is more prone to significant interactions. This is due to its effect on various enzymes involved in drug metabolism, requiring careful consideration when prescribing.
Side Effects
While both medications can cause side effects like nausea and headache, Itraconazole is associated with more serious risks, such as heart failure and liver damage, in some patients.
Fluconazole Advantages
Suitable Conditions
Fluconazole is particularly effective for treating Candida infections, including thrush and vaginal yeast infections. Its excellent oral absorption makes it a convenient option.
Patient Compatibility
Due to its favorable side effect profile and fewer drug interactions, Fluconazole is often preferred for patients who are on multiple medications or have mild fungal infections.
Itraconazole Advantages
Suitable Conditions
Itraconazole stands out for its effectiveness against a broad range of fungal infections. It’s particularly valuable in treating conditions like:
- Aspergillosis: Targets Aspergillus fungi, which can cause serious respiratory issues.
- Blastomycosis and Histoplasmosis: Treats systemic fungal infections that can affect multiple organs.
- Onychomycosis: Effective for nail fungus, offering a solution for both fingernail and toenail infections.
Patient Compatibility
Itraconazole is a preferred choice for patients requiring treatment for fungi not susceptible to Fluconazole. Its ability to target a wider variety of fungi makes it suitable for complex or resistant fungal infections.
Choosing Between Fluconazole and Itraconazole
Factors to Consider
When deciding between Fluconazole and Itraconazole, consider:
- Type of fungal infection: Specific fungi may respond better to one drug.
- Patient health: Underlying conditions and overall health can influence the choice.
- Drug interactions: Consider other medications the patient is taking.
- Side effects: Evaluate the risk and severity of potential side effects.
Doctor’s Role in Selection
Doctors play a crucial role in determining the best antifungal medication. They will assess the infection type, patient history, and medication interactions to make an informed decision, ensuring the chosen treatment aligns with the patient’s specific needs.
Side Effects and Safety
Common Side Effects of Fluconazole
Fluconazole can cause side effects such as:
- Nausea and vomiting
- Headache
- Dizziness
- Stomach pain
Common Side Effects of Itraconazole
Itraconazole may lead to:
- Nausea and vomiting
- Headache
- Rash
- Elevated liver enzymes, potentially signaling liver damage
Safety Precautions and Warnings
Both medications require careful monitoring for side effects and interactions. Liver function tests may be necessary due to the risk of liver damage. Patients with existing heart conditions should exercise caution with Itraconazole due to potential heart-related side effects.
Drug Interactions
Major Interactions with Fluconazole
Fluconazole can interact with drugs like:
- Warfarin: Increased risk of bleeding.
- Certain antibiotics and antivirals: May increase medication levels, raising side effects.
Major Interactions with Itraconazole
Itraconazole’s interactions include:
- Blood pressure medications: Can cause blood pressure to drop too low.
- Statins: Increased risk of muscle damage.
How to Manage Drug Interactions
To manage interactions, healthcare providers may:
- Adjust dosages: Modifying doses to prevent interaction effects.
- Monitor closely: More frequent monitoring for signs of interaction.
- Alternative medications: Switching to other medications when necessary.
Patient Considerations
When to Prefer Fluconazole
Choose Fluconazole for:
- Candida infections: Such as thrush and vaginal yeast infections.
- Patients with potential heart issues: Due to fewer heart-related side effects.
When to Prefer Itraconazole
Opt for Itraconazole for:
- Resistant fungal infections: Not responsive to Fluconazole.
- Complex systemic infections: Like aspergillosis, blastomycosis, and histoplasmosis.
Monitoring and Follow-Up
Regular follow-up appointments are crucial to monitor the treatment’s effectiveness and side effects. Adjustments to the treatment plan, including changing medications or dosages, may be necessary based on the patient’s response and any emerging side effects.
Frequently Asked Questions
What is Fluconazole primarily used for?
Fluconazole is primarily used to treat and prevent a wide range of fungal infections, including yeast infections like oral thrush and vaginal candidiasis. It’s particularly favored for its effectiveness against Candida species, making it a go-to option for infections in various parts of the body.
How does Itraconazole work?
Itraconazole works by inhibiting the synthesis of ergosterol, a crucial component of fungal cell membranes. This disruption leads to a weakening and eventual breakdown of the fungal cell membrane, effectively eradicating the infection. Its broad spectrum makes it effective against a wide variety of fungi.
Can Fluconazole and Itraconazole be taken together?
Typically, Fluconazole and Itraconazole are not taken together due to potential drug interactions and overlapping side effects. Combining them could increase the risk of liver damage and other adverse effects. It’s essential to follow a healthcare provider’s guidance when taking any antifungal medications.
What are the major differences between Fluconazole and Itraconazole?
The major differences between Fluconazole and Itraconazole include their chemical structure, spectrum of activity, and absorption/metabolism properties. Fluconazole is better absorbed, has fewer drug interactions, and is typically used for Candida infections. Itraconazole has a broader spectrum, making it effective against a wider range of fungi but comes with more potential for drug interactions.
Conclusion
The distinction between Fluconazole and Itraconazole marks a critical consideration in the treatment of fungal infections. By understanding their differences, healthcare professionals can tailor treatments to suit individual patient needs, optimizing outcomes while minimizing risks. These medications represent powerful tools in the fight against fungal infections, and their effective use is a testament to the advancements in antifungal therapy.
Choosing the right antifungal medication requires a comprehensive understanding of the patient’s specific condition, potential drug interactions, and the unique properties of each medication. With the right approach, the selection between Fluconazole and Itraconazole can be made confidently, ensuring effective and safe treatment of fungal infections.