Bacteria are a vast and diverse group of organisms that play crucial roles in the ecosystem and human health. Differentiating between types, such as E. coli and Serratia marcescens, is vital for understanding their impacts and managing their effects. Both bacteria are common in various environments but have distinct characteristics and behaviors.
E. coli (Escherichia coli) and Serratia marcescens differ primarily in their habitat preferences, pathogenic capabilities, and physiological traits. E. coli is famously known for its presence in the intestines of humans and animals and its role in foodborne illness. In contrast, Serratia marcescens is notorious for its role in hospital-acquired infections and its distinctive red pigment production under certain conditions.
These bacteria are not only differentiated by their genetic makeup but also by their environmental adaptations and the different health implications they carry. Distinguishing between these two helps in medical diagnostics and treatment planning, especially in preventing and controlling infections in healthcare settings.

E. coli Overview
Basic Characteristics
Escherichia coli, commonly known as E. coli, is a rod-shaped bacterium that is a crucial member of the gut microbiota in humans and warm-blooded animals. Its ability to ferment lactose efficiently at 37°C distinguishes it from many other intestinal bacteria. Most strains of E. coli are harmless and serve vital roles in the digestive system, such as aiding in the breakdown of food and the absorption of nutrients. However, certain strains can be pathogenic, leading to food poisoning and severe gastrointestinal diseases.
Common Habitats
E. coli naturally resides in the intestines of healthy people and animals. Beyond the gut, it can be found in environments contaminated with fecal matter, including rivers, lakes, and soil. This bacterium is also a common occupant in raw meats, particularly ground beef, and improperly prepared or stored food products. Due to its prevalence in fecal material, E. coli serves as an indicator organism to test the effectiveness of water treatment and the presence of fecal contamination.
Serratia Marcescens Basics
Defining Features
Serratia marcescens is notable for its distinct red pigment, prodigiosin, which it produces at room temperature under certain conditions. This pigment is not just a hallmark for identification but also has been studied for its antimicrobial and anticancer properties. Serratia marcescens is inherently resistant to several antibiotics and has enzymes capable of degrading a variety of harmful substances, making it a robust bacterium in hostile environments.
Natural Environments
Unlike E. coli, which thrives primarily within the gastrointestinal tract, Serratia marcescens is found in a wider range of moist environments. These include soil, water, and plants. It is also commonly found in bathrooms and other damp areas inside homes and hospitals, where it can colonize sinks, tiles, and shower curtains. Its resilience and adaptability to diverse environments make it a frequent cause of hospital-acquired infections.
Comparative Analysis
Morphology and Structure
Both E. coli and Serratia marcescens are rod-shaped and gram-negative, which means they both have a thin peptidoglycan layer and an outer membrane containing lipopolysaccharides. Under the microscope, E. coli cells typically appear as shorter rods, while Serratia marcescens can form longer and sometimes filamentous rods. The red pigment of Serratia marcescens under stress or nutrient-limited conditions is a key differentiator from the typically non-pigmented E. coli.
Genetic Differences
The genetic makeup of these two bacteria reveals significant differences in their capabilities and effects. E. coli’s genome has been extensively studied, providing insights into its versatile metabolism and the genetic basis for its pathogenic strains. On the other hand, the genome of Serratia marcescens encodes a wider array of enzymes that confer resistance to antibiotics and enable it to degrade diverse substances, contributing to its survival in various environments.
Growth Conditions
Optimal Growth Temperatures
E. coli grows best at human body temperature, around 37°C, aligning with its natural habitat in the human gut. Serratia marcescens, however, can thrive at a broader range of temperatures, often between 25°C and 30°C, which suits its more diverse environments.
pH and Oxygen Requirements
E. coli prefers a neutral to slightly acidic environment (pH 6-7) and is facultatively anaerobic, meaning it can grow without oxygen but performs best with it. Serratia marcescens also grows well under facultatively anaerobic conditions but can tolerate a wider range of pH levels, from slightly acidic to slightly alkaline. This adaptability helps Serratia marcescens colonize more varied environments compared to E. coli.
Pathogenicity and Health Impacts
E. coli Pathogenic Strains
Among the diverse strains of E. coli, several are notorious for their pathogenic effects on humans. These strains are categorized based on the nature of the diseases they cause:
- Enterotoxigenic E. coli (ETEC): Often called the cause of traveler’s diarrhea, ETEC produces toxins that stimulate the lining of the intestines, leading to diarrhea.
- Enteropathogenic E. coli (EPEC): Commonly affects infants, leading to watery diarrhea and fever without producing toxins.
- Enterohemorrhagic E. coli (EHEC), particularly the O157:H7 strain: Causes severe abdominal cramps, bloody diarrhea, and occasional kidney failure, known as hemolytic uremic syndrome.
These pathogenic strains can contaminate water and food sources, making them major public health concerns. Their presence in undercooked meats, especially beef, and improperly washed vegetables can lead to outbreaks of gastrointestinal diseases.
Serratia Marcescens and Disease
Serratia marcescens is primarily associated with hospital-acquired infections (HAIs), where it exploits the weakened immune systems of hospitalized patients. Common infections include:
- Pneumonia and respiratory tract infections: Occur when the bacteria enter through devices like ventilators or breathing tubes.
- Urinary tract infections: Develop from the use of catheters.
- Wound infections: Follow surgical procedures or catheter insertions.
The bacterium’s ability to form biofilms on medical devices significantly contributes to its virulence and resilience against treatments.
Laboratory Identification
Culturing Techniques
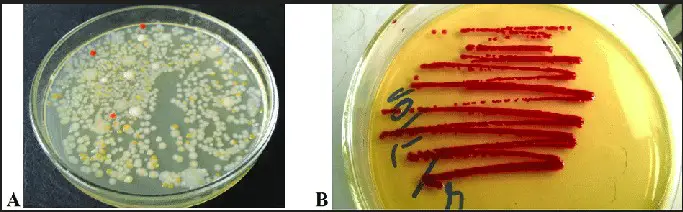
Culturing is essential for identifying and studying both E. coli and Serratia marcescens. The key steps include:
- Sample collection: Obtaining specimens from the suspected infection site.
- Media selection: Using specific growth media like MacConkey agar for E. coli, which turns pink due to lactose fermentation, and blood agar for Serratia marcescens, which may show red pigment production.
- Incubation: Cultures are incubated at optimal temperatures to promote growth; typically, 37°C for E. coli and 25°C to 30°C for Serratia marcescens.
Biochemical Tests
Biochemical tests further differentiate these bacteria based on their metabolic capabilities:
- IMViC tests: Separate E. coli (positive for indole and methyl red tests) from other Enterobacteriaceae.
- DNase test: Serratia marcescens is positive, indicating its ability to degrade DNA.
Antibiotic Resistance
E. coli Resistance Mechanisms
Antibiotic resistance in E. coli is a growing concern, particularly with the spread of Extended Spectrum Beta-Lactamases (ESBL) and carbapenemases, enzymes that break down a wide range of beta-lactam antibiotics. Factors contributing to resistance include:
- Genetic mutations: Spontaneous changes in DNA that confer resistance.
- Horizontal gene transfer: Acquisition of resistance genes from other bacteria.
Serratia Marcescens Defense
Serratia marcescens exhibits resistance to multiple antibiotics, largely through:
- Production of carbapenemases: These enzymes provide resistance to carbapenems, one of the last lines of defense in antibiotic treatments.
- Efflux pumps: Remove antibiotics from bacterial cells before they can be effective.
Industrial and Medical Uses
E. coli in Biotechnology
E. coli’s well-understood genetics make it an ideal tool in biotechnology, used for:
- Protein production: E. coli is used to synthesize insulin and other important proteins.
- Genetic studies: As a model organism in genetic research, aiding in understanding bacterial physiology and genetics.
Serratia Marcescens Applications
Despite its pathogenic nature, Serratia marcescens has beneficial applications, including:
- Enzyme production: Produces enzymes like prodigiosin with potential applications in cancer therapy.
- Bioremediation: Capable of degrading hazardous substances, thus useful in environmental cleanup.
Frequently Asked Questions
What is E. coli?
E. coli, or Escherichia coli, is a bacterium commonly found in the intestines of humans and warm-blooded animals. While most strains are harmless, some can cause severe food poisoning, urinary tract infections, and other illnesses.
How does Serratia marcescens affect humans?
Serratia marcescens is an opportunistic pathogen known for causing nosocomial infections such as pneumonia, urinary tract infections, and wound infections, particularly in immunocompromised individuals.
Can E. coli and Serratia marcescens be found in the same environments?
While both bacteria can be present in similar environments such as water and soil, E. coli is predominantly found in the intestines of animals and humans, whereas Serratia marcescens is more commonly associated with moist environments and can also colonize man-made water reservoirs.
How are E. coli and Serratia marcescens identified in the laboratory?
Both bacteria can be identified through selective culturing techniques and biochemical tests which differentiate their unique characteristics, such as lactose fermentation by E. coli and red pigment production by Serratia marcescens.
What are the key differences in antibiotic resistance between E. coli and Serratia marcescens?
E. coli and Serratia marcescens have shown varying degrees of resistance to antibiotics. E. coli is particularly known for its resistance to commonly used antibiotics like ampicillin, while Serratia marcescens exhibits resistance mechanisms that can break down a broader range of antibiotics.
Conclusion
Understanding the differences between E. coli and Serratia marcescens is crucial for effective clinical management and infection control. These distinctions not only help in pinpointing the source of infections but also guide treatment decisions, especially in an era of rising antibiotic resistance. Recognizing their unique characteristics enables healthcare providers to implement targeted interventions that can significantly reduce healthcare-associated infections.
In summary, while both bacteria share common environments, their impact on human health varies greatly, necessitating distinct approaches in medical and environmental microbiology. This knowledge not only aids in scientific research but also enhances public health strategies by informing better hygiene and safety protocols.

