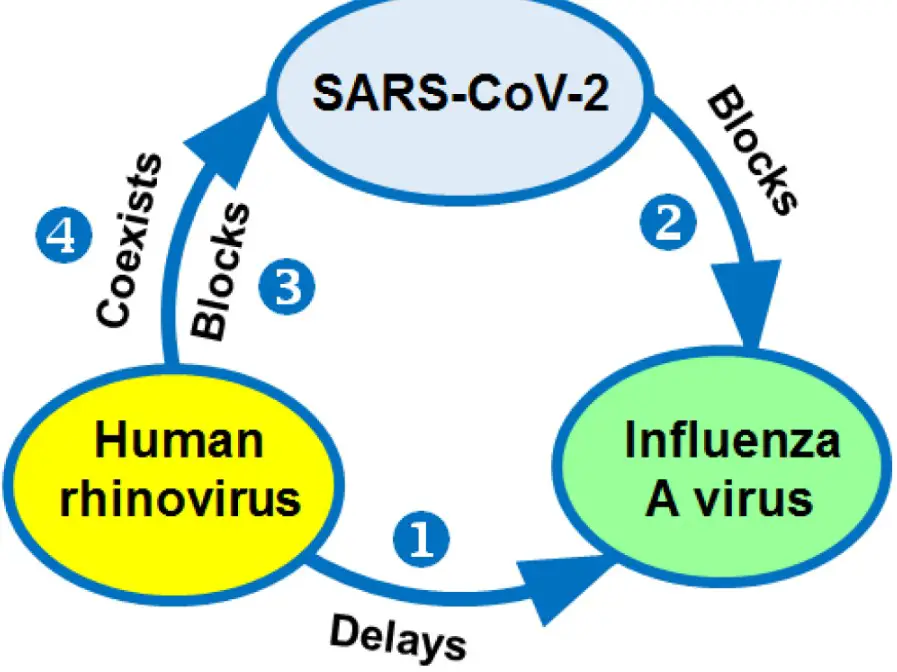
Respiratory viruses are a leading cause of illness globally, with the Coronavirus and Rhinovirus being two prominent examples. Each virus contributes significantly to respiratory infections, affecting millions of individuals annually. Despite their common target—the respiratory system—their characteristics, impact, and management strategies differ considerably.
The key difference between Coronavirus and Rhinovirus lies in their structure, modes of transmission, and the severity of the diseases they cause. Coronavirus, a larger family of viruses, is known for causing illnesses ranging from the common cold to more severe diseases such as COVID-19. Rhinovirus, on the other hand, is primarily associated with the common cold and exhibits a different set of symptoms and transmission methods.
Both viruses play critical roles in public health concerns, leading to significant morbidity and mortality rates worldwide. The distinction between them extends beyond their biological makeup to include their epidemiological impacts and the strategies developed to combat their spread. Understanding these differences is vital for effective prevention, diagnosis, and treatment of the infections they cause.
Viral Structures
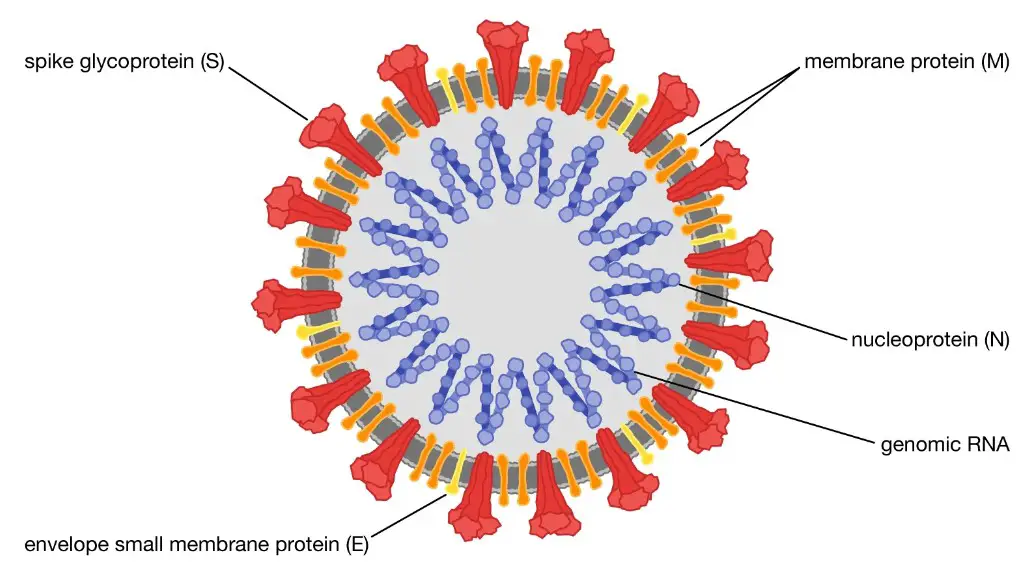
Coronavirus Characteristics
The Coronavirus family, named for its crown-like appearance under a microscope, possesses a single-stranded RNA as its genetic material, enclosed within a spherical envelope. This envelope is studded with spike proteins that facilitate entry into host cells. These spike proteins are critical for the virus’s ability to infect and are the target of many vaccines. The size of Coronaviruses ranges from approximately 80 to 120 nanometers in diameter, making them one of the larger viruses affecting humans.
Rhinovirus Characteristics
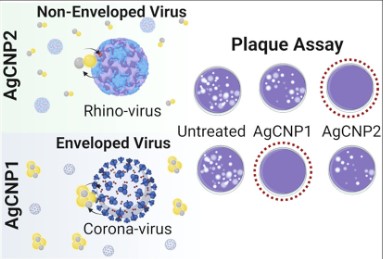
In contrast, Rhinoviruses are smaller, with no outer envelope, and contain single-stranded RNA. They measure about 30 nanometers across and possess a capsid made of protein that encases their genetic material. Unlike Coronaviruses, Rhinoviruses do not have spike proteins but use other mechanisms to attach to and enter host cells. Their smaller size and lack of an envelope contribute to their resilience in the external environment, aiding their transmission.
Comparison of Structural Differences
The main structural differences between the two viruses lie in their size, presence or absence of an envelope, and the mechanisms of cell entry. These differences not only affect how these viruses are transmitted but also influence the development of treatments and vaccines. For instance, the enveloped nature of Coronaviruses makes them more susceptible to disinfectants and environmental factors, whereas the non-enveloped Rhinoviruses are more resilient in various conditions.
Transmission Modes
How Coronavirus Spreads
Coronavirus primarily spreads through respiratory droplets when an infected person coughs, sneezes, or talks. These droplets can be inhaled by people nearby or land on surfaces that others may touch, subsequently transferring the virus when they touch their face. Airborne transmission, involving smaller droplet nuclei that can remain suspended in the air for hours, is also a significant concern in enclosed spaces with inadequate ventilation.
Rhinovirus Transmission
Rhinovirus spreads mostly through direct contact with infected persons or contaminated surfaces. Touching one’s nose or eyes after touching a surface contaminated with the Rhinovirus can lead to infection. While respiratory droplets also play a role in its spread, the direct contact route is more common for Rhinoviruses due to their structural resilience.
Differences in Transmission Mechanisms
The key differences in transmission between the two viruses are related to the environments they thrive in and the routes through which they infect hosts. Coronaviruses, with their ability to spread via airborne droplets, pose a higher risk in crowded and poorly ventilated spaces. Rhinoviruses, although capable of airborne spread, are more often transmitted through physical contact, making hand hygiene a critical preventive measure.
Symptoms and Severity
Common Symptoms of Coronavirus
Infections with Coronavirus can range from mild symptoms similar to the common cold to severe respiratory conditions like pneumonia. Common symptoms include:
- Fever
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
Severe cases, especially in vulnerable populations, can lead to significant health complications, including death.
Typical Rhinovirus Symptoms
Rhinovirus infections typically result in milder symptoms that include:
- Runny or stuffy nose
- Sore throat
- Cough
- Sneezing
- Mild headache
- Body aches
Symptoms usually resolve on their own within a week or so, without leading to severe health issues.
Comparing Symptom Severity and Progression
While both viruses can cause respiratory symptoms, the severity and progression of illnesses they cause differ significantly. Coronavirus infections can lead to severe and life-threatening diseases, particularly in the elderly or those with underlying health conditions. Rhinovirus, meanwhile, tends to cause less severe symptoms that are typically confined to the upper respiratory tract.
Risk Factors
Coronavirus Risk Groups
Certain groups are more at risk of experiencing severe outcomes from Coronavirus infection. These include:
- Older adults
- People with underlying medical conditions (like heart disease, diabetes, or lung disease)
- Those with weakened immune systems
Rhinovirus Susceptibility
Rhinovirus infections do not typically discriminate by age or health status but can be more problematic for:
- Asthmatics
- Individuals with chronic obstructive pulmonary disease (COPD)
- Those with compromised immune systems, although the risk of severe disease is much lower than with Coronavirus
Contrasting the Risk Factors
The risk factors for severe disease differ between the two viruses, with Coronavirus posing a significant risk to a broader section of the population, including healthy individuals, if not managed properly. Rhinovirus, while infectious and capable of causing discomfort, generally does not result in severe health complications except in those with pre-existing respiratory conditions.
Diagnostic Methods
Testing for Coronavirus
Testing is crucial for controlling the spread of Coronavirus. The primary method is the RT-PCR test, which detects the virus’s genetic material in respiratory specimens. Another quick method is the antigen test that looks for specific proteins from the virus. Both tests require samples usually taken from a nasal or throat swab.
Steps involved in RT-PCR testing:
- Collection of a nasal or throat swab.
- Extraction of viral RNA from the sample.
- Amplification of the RNA and detection using RT-PCR technology.
- Interpretation of results by healthcare professionals.
Antibody tests can also identify people who have been infected in the past but are less useful for diagnosing current infections.
Rhinovirus Detection Techniques
Rhinovirus detection is not commonly performed for clinical diagnosis due to the mild nature of the illness. However, when needed, RT-PCR is also the standard test for identifying Rhinovirus infections, similar to Coronavirus testing. The process involves detecting the genetic material of the Rhinovirus in respiratory secretions.
Differences in Diagnosis Processes
The main difference in diagnosis processes lies in the frequency and purpose of testing. Coronavirus testing is widespread due to its public health implications, including contact tracing and isolation measures. Rhinovirus testing, on the other hand, is less common and usually reserved for research purposes or in cases where a more precise diagnosis may influence patient management, particularly in individuals with severe respiratory diseases or immune deficiencies.
Treatment Options
Coronavirus Treatments
Treatment for Coronavirus infection varies depending on the severity of the symptoms. For mild cases, treatment involves rest, hydration, and over-the-counter medications to relieve symptoms. Moderate to severe cases may require hospitalization and can include:
- Antiviral drugs like Remdesivir.
- Steroids to reduce inflammation.
- Oxygen therapy for respiratory support.
- Monoclonal antibodies and convalescent plasma therapy in some cases.
Vaccination is the cornerstone of Coronavirus prevention and management.
Managing Rhinovirus Infections
Treatment for Rhinovirus infections is primarily supportive, focusing on relieving symptoms since the infection typically resolves on its own. Recommendations include:
- Adequate rest.
- Increased fluid intake.
- Use of over-the-counter pain relievers and decongestants.
There are no specific antiviral drugs for Rhinovirus due to its high mutation rate and the mild nature of the disease.
Treatment Effectiveness and Availability
While treatments for both viruses aim to relieve symptoms and prevent complications, Coronavirus treatments and vaccines are more critical due to the virus’s potential to cause severe disease and global health impact. The availability of effective vaccines against Coronavirus has significantly changed the course of the pandemic, highlighting differences in treatment approaches and their effectiveness.
Prevention Strategies
Preventing Coronavirus Exposure
Preventing Coronavirus involves a multi-layered approach:
- Wearing masks in public spaces.
- Maintaining social distance.
- Practicing hand hygiene.
- Vaccination.
These measures reduce the risk of airborne and droplet transmission.
Rhinovirus Prevention Measures
Rhinovirus prevention focuses on personal hygiene:
- Regular hand washing.
- Avoiding touching the face with unwashed hands.
- Staying away from infected individuals.
Comparative Analysis of Prevention Techniques
The prevention strategies for both viruses share common elements, such as the importance of hand hygiene. However, the emphasis on mask-wearing and vaccination is particularly pronounced for Coronavirus due to its higher transmission rate and severity of illness. The widespread adoption of vaccines has been a game-changer in managing Coronavirus spread, a strategy not applicable to Rhinovirus because of its diverse strains and mild impact.
Impact on Public Health
Global Impact of Coronavirus
The global impact of Coronavirus has been profound, affecting every aspect of society. The pandemic led to unprecedented public health measures, including lockdowns, travel restrictions, and the acceleration of vaccine development. The economic, social, and mental health repercussions have been significant, making it a primary focus for governments and health organizations worldwide.
Rhinovirus and Public Health
While Rhinovirus is the most common cause of the common cold, its impact on public health is significantly less severe compared to Coronavirus. It does contribute to economic costs related to lost productivity and healthcare visits, but it does not necessitate the same level of public health response.
Contrasting the Health Care Responses
The health care response to Coronavirus has involved large-scale public health initiatives, including testing, contact tracing, and mass vaccination campaigns. For Rhinovirus, the response is more focused on individual behavior changes to prevent spread, without the need for large-scale public health measures. This difference highlights the varied impact these viruses have on society and the necessity of tailored public health strategies to manage them effectively.
FAQs
How are Coronavirus and Rhinovirus transmitted?
Coronavirus is primarily transmitted through respiratory droplets when an infected person coughs or sneezes. It can also spread by touching surfaces contaminated with the virus. Rhinovirus spreads similarly but is more adept at transmission through direct contact with contaminated surfaces or personal contact, such as shaking hands.
Can Rhinovirus and Coronavirus cause similar symptoms?
Yes, both viruses can cause similar symptoms, including coughing, sneezing, a sore throat, and fever. However, Coronavirus infections can lead to more severe respiratory illnesses like pneumonia, particularly in vulnerable populations, whereas Rhinovirus infections tend to result in milder, common cold-like symptoms.
Are there vaccines available for both viruses?
Currently, vaccines are available for various strains of Coronavirus, most notably for SARS-CoV-2, the virus responsible for COVID-19. There are no vaccines for Rhinovirus due to its high mutation rate and the existence of numerous strains, making vaccine development challenging.
How can we differentiate between a Coronavirus and a Rhinovirus infection?
Differentiating between Coronavirus and Rhinovirus infections primarily involves laboratory testing. PCR tests are commonly used to detect the presence of SARS-CoV-2, the virus causing COVID-19. Other diagnostic tests may be employed to identify Rhinovirus infections, though such differentiation often relies on evaluating symptoms and exposure history as well.
Conclusion
Understanding the difference between Coronavirus and Rhinovirus is crucial for managing respiratory infections effectively. These viruses, while sharing similarities in the symptoms they produce, differ significantly in their severity, transmission, and the global impact they have on health systems. Recognizing these distinctions not only aids in the accurate diagnosis and treatment of infections but also informs public health strategies aimed at preventing their spread.
As we continue to navigate through the challenges posed by respiratory viruses, it becomes increasingly important to remain vigilant and informed. By adopting appropriate preventive measures, staying updated on the latest research, and supporting vaccination efforts where available, we can mitigate the impact of these viruses on our communities and health systems.