Antibodies are crucial components of the immune system, acting as the body’s defense mechanism against foreign invaders such as viruses and bacteria. These Y-shaped proteins identify and neutralize pathogens, showcasing the immune system’s precision and adaptability. However, not all antibodies operate in the same way, leading to a distinction between complete and incomplete antibodies. This differentiation is not just academic; it has significant implications for how we understand and manage immune responses.
Complete antibodies, also known as IgG and IgM, can directly bind to antigens and cause visible agglutination, facilitating the immune system’s ability to target and eliminate pathogens. Incomplete antibodies, such as IgA, IgD, and IgE, bind to antigens but do not cause visible agglutination. Instead, they serve unique roles, like crossing placental barriers or triggering allergic reactions, highlighting the diverse tactics employed by the immune system to protect the body.
Understanding the difference between complete and incomplete antibodies is crucial for diagnosing diseases, developing vaccines, and crafting therapeutic strategies. These distinctions help medical professionals and researchers tailor treatments and diagnostics, ensuring that interventions are as effective as possible. With ongoing research, the knowledge about these antibodies continues to evolve, promising more sophisticated approaches to combating diseases.
What are Antibodies?
Definition and Function
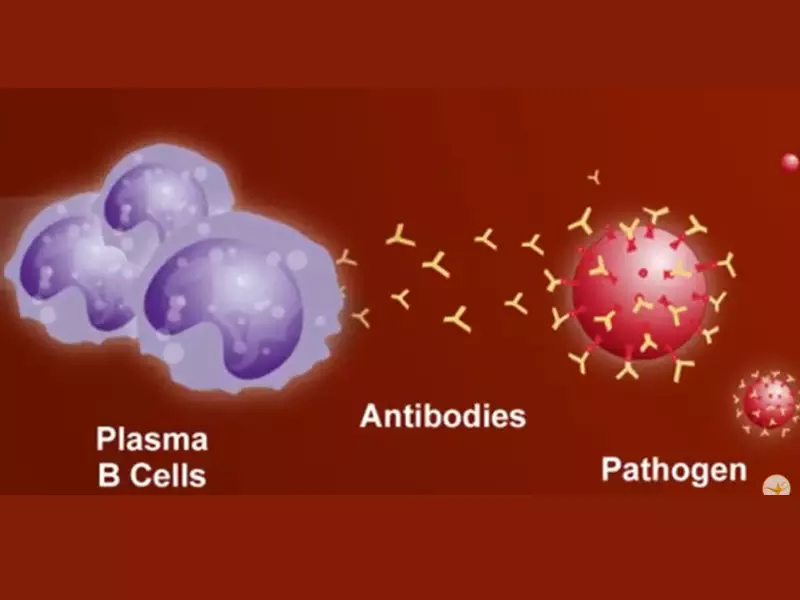
Antibodies are proteins produced by the immune system to identify and neutralize foreign objects such as bacteria and viruses. Each antibody recognizes a specific antigen unique to its target, making the immune response both precise and adaptable. The primary function of antibodies includes:
- Binding to antigens to neutralize pathogens or mark them for destruction by other immune cells.
- Facilitating phagocytosis, where pathogens coated with antibodies are more easily engulfed and destroyed by phagocytes.
- Triggering the complement system, a series of proteins that assists in destroying pathogens.
Role in the Immune System
Antibodies play a pivotal role in the immune system, operating as both defenders and signalers. They are key players in the adaptive immune response, which learns and remembers previous encounters with pathogens, ensuring a faster and more effective response upon subsequent exposures. Their roles include:
- Direct neutralization of pathogens, preventing them from entering or damaging healthy cells.
- Opsonization, where antibodies tag pathogens for elimination.
- Activation of the complement system to further attack the pathogen.
Complete Antibodies
Description
Complete antibodies are capable of binding directly to antigens and can cause visible agglutination (clumping of particles). This group includes antibodies like IgG and IgM, known for their effectiveness in targeting and neutralizing a wide range of pathogens.
Characteristics
These antibodies share several key characteristics:
- Ability to cross-link antigens, leading to agglutination.
- Presence in various body fluids, providing widespread immune defense.
- IgG can cross the placental barrier, providing newborns with passive immunity.
Types and Examples
- IgG: The most abundant in the body, effective against bacteria, viruses, and toxins.
- IgM: The first antibody type produced in response to an infection.
How They Work in the Immune Response
Complete antibodies function through several mechanisms:
- Neutralization: Blocking the biological effects of pathogens.
- Opsonization: Enhancing phagocytosis of antigens.
- Complement activation: Leading to the destruction of the pathogen.
Incomplete Antibodies
Description
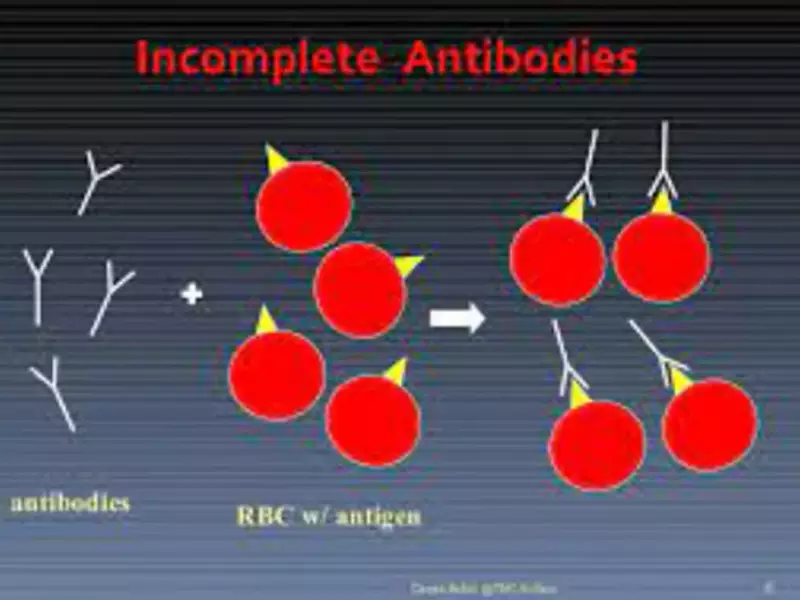
Incomplete antibodies, such as IgA, IgD, and IgE, do not cause visible agglutination when they bind to antigens. Their actions are more subtle but vital in specific contexts, such as mucosal immunity or allergic responses.
Characteristics
- Location-specific: Found in places like the respiratory and digestive tracts (IgA).
- Function-specific: Each plays a role tailored to its environment, like IgE in allergic reactions.
Types and Examples
- IgA: Protects body surfaces exposed to foreign substances.
- IgD: Acts mainly as an antigen receptor on B cells.
- IgE: Involved in allergic reactions and protection against parasites.
Role in Immune System Without Visible Agglutination
Incomplete antibodies contribute to the immune response by:
- Signaling: Alerting immune cells to the presence of a pathogen.
- Blocking: Preventing pathogens from entering or damaging cells.
- Modulating: Adjusting the immune response to be more effective against specific threats.
Key Differences
Binding to Antigens
Complete antibodies and incomplete antibodies differ fundamentally in how they interact with antigens. Complete antibodies can directly bind to antigens and form visible clusters known as agglutination. This reaction is crucial for the immune system to easily identify and eliminate pathogens. In contrast, incomplete antibodies also bind to antigens but do not cause agglutination, playing a more subtle role in the immune response.
Visibility of Reaction
The visibility of the immune reaction is a clear distinction between these two types of antibodies. With complete antibodies, the agglutination is a visible sign of the immune system’s response, making it easier to identify and study in laboratory settings. Incomplete antibodies, however, work behind the scenes, with their effects often requiring more sophisticated methods to observe.
Mechanism of Action
The mechanism of action also sets complete and incomplete antibodies apart. Complete antibodies can neutralize pathogens, promote phagocytosis, and activate complement systems directly through their ability to bind and cluster antigens. Incomplete antibodies, while unable to cause agglutination, still play critical roles in immune defense through other mechanisms, such as blocking pathogen entry into cells or triggering specific immune cells.
Clinical Implications
Understanding the differences between complete and incomplete antibodies has significant clinical implications. The way these antibodies interact with antigens affects vaccine development, therapeutic strategies, and disease diagnosis. For example, vaccines might be designed to elicit a strong response from complete antibodies, while certain therapies might aim to modulate the activity of incomplete antibodies for diseases like allergies or autoimmune disorders.
Clinical Significance
Complete Antibodies
Diagnostic Uses
Complete antibodies, especially IgG, are widely used in diagnostic tests to detect the presence of specific pathogens or to confirm a past infection. Their ability to agglutinate makes them ideal markers in tests such as ELISA (enzyme-linked immunosorbent assay) and Rapid diagnostic tests (RDTs).
Therapeutic Applications
Therapeutic applications of complete antibodies include the use of monoclonal antibodies in treating various diseases, ranging from cancers to autoimmune diseases. These treatments often leverage the ability of complete antibodies to target and neutralize specific pathogens or diseased cells.
Incomplete Antibodies
Diagnostic Challenges
The subtle nature of incomplete antibodies presents diagnostic challenges. Their inability to cause agglutination means that alternative methods must be used to detect their presence or measure their levels, requiring more sophisticated and sensitive diagnostic tools.
Research and Therapeutic Potential
The research and therapeutic potential of incomplete antibodies is immense, particularly in areas like allergy treatment, where IgE’s role is critical. Understanding how these antibodies operate could lead to new ways to prevent or treat allergic reactions or improve mucosal immunity with targeted IgA therapies.
Testing and Detection
Techniques for Identifying Complete Antibodies
To identify complete antibodies, several techniques are employed, reflecting their ability to agglutinate antigens. These include:
- Agglutination tests: Used for blood typing and detecting infections.
- ELISA: Useful for quantifying specific antibodies in the blood.
- Western blotting: Helps confirm the presence of antibodies following an ELISA test.
Methods for Detecting Incomplete Antibodies
Detecting incomplete antibodies requires more nuanced techniques, given their lack of visible agglutination. Methods include:
- Indirect immunofluorescence: Allows for the detection of antibodies bound to antigens on a cell’s surface or within tissues.
- Flow cytometry: Can measure the presence and quantity of antibodies bound to antigens on the surface of cells.
- Radioimmunoassays (RIA) and immunoprecipitation: Techniques for detecting and measuring antibodies in the blood.
Importance in Medical Diagnostics
The ability to accurately detect both complete and incomplete antibodies is vital in medical diagnostics. It enables the identification of current or past infections, assessment of immune status, and helps guide treatment decisions. Advanced testing techniques are continually being developed and refined to improve the sensitivity and specificity of antibody detection, illustrating the ongoing importance of understanding these immune system components in clinical settings.
FAQs
What are Complete Antibodies?
Complete antibodies, primarily IgG and IgM, have the ability to directly bind to antigens and cause visible agglutination. This property is essential for the effective neutralization and removal of pathogens from the body, playing a crucial role in the immune response.
How do Incomplete Antibodies Function?
Incomplete antibodies, such as IgA, IgD, and IgE, bind to antigens but do not cause agglutination. They perform specialized functions, including mucosal defense (IgA), antigen receptor roles (IgD), and triggering allergic reactions (IgE), contributing to a comprehensive immune defense strategy.
Why is the Distinction Between Complete and Incomplete Antibodies Important?
The distinction between complete and incomplete antibodies is vital for diagnostics and therapy. It influences how diseases are detected and managed, affecting vaccine development and the creation of targeted treatments that leverage the unique properties of each antibody type.
Can Incomplete Antibodies Cross the Placental Barrier?
Incomplete antibodies typically do not cross the placental barrier. This function is primarily attributed to IgG, a type of complete antibody, which can provide passive immunity to the fetus by transferring maternal antibodies.
Conclusion
The nuanced differences between complete and incomplete antibodies underscore the complexity of the immune system and its myriad strategies for defending against pathogens. These distinctions are not just of academic interest; they have practical implications for diagnostics, treatment, and our overall understanding of immunology. As research progresses, our comprehension of these antibodies will deepen, paving the way for more effective medical interventions and a greater appreciation of the immune system’s versatility.
The exploration of complete and incomplete antibodies represents a fascinating facet of immunology, one that highlights the elegance and sophistication of the body’s defense mechanisms. By continuing to study these differences, scientists and medical professionals can develop more precise diagnostic tools and therapies, ultimately leading to better health outcomes and a deeper understanding of human biology.
