Angiotensin, a peptide hormone, plays a crucial role in the regulation of blood pressure and fluid balance within the body. This hormone system, integral to the cardiovascular system’s function, operates through various forms, primarily angiotensin I and II. Each form carries specific responsibilities and effects that are vital for maintaining circulatory stability and responding to the body’s changing needs.
Angiotensin I and II are distinct entities with unique functions and impacts on the body. Angiotensin I, a decapeptide, serves as a precursor that is converted into angiotensin II, an octapeptide, through the action of angiotensin-converting enzyme (ACE). While angiotensin I has minimal direct biological activity, angiotensin II acts as a potent vasopressor and stimulates aldosterone secretion, significantly influencing blood pressure regulation and fluid balance.
The differences between angiotensin I and II extend beyond their structure and conversion process. Angiotensin II’s ability to bind to receptors throughout the body initiates a cascade of physiological effects, including vasoconstriction and water retention, crucial for blood pressure management and cardiovascular health. This detailed examination sheds light on their pivotal roles and underscores the complexity of the body’s regulatory mechanisms.
Angiotensin Overview
What is Angiotensin?
Angiotensin is a peptide hormone that plays a crucial role in regulating blood pressure and fluid balance in the body. It is part of a complex system that ensures our cardiovascular health is maintained, responding dynamically to the body’s needs. The significance of angiotensin lies in its ability to influence various physiological processes, making it a cornerstone of cardiovascular function.
Role in Blood Pressure Regulation
Angiotensin significantly impacts blood pressure control. It does so by affecting blood vessel constriction and influencing the volume of fluids in the body. The system that manages angiotensin production, the renin-angiotensin system (RAS), activates in response to low blood pressure, leading to increased levels of angiotensin, which in turn raises blood pressure.
Connection to the Renin-Angiotensin System
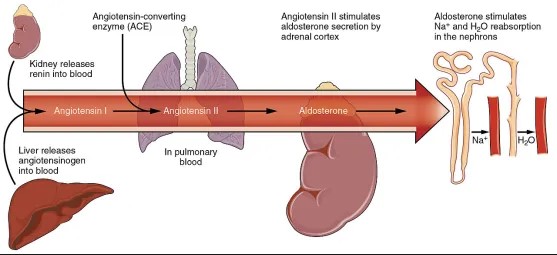
The renin-angiotensin system is essential for cardiovascular health. Renin, an enzyme, starts the process by converting angiotensinogen (a precursor protein) into angiotensin I. This is the beginning of a chain reaction that leads to the production of angiotensin II, the most active form, which has direct effects on blood pressure regulation.
Types of Angiotensin
Brief on Various Forms
Angiotensin exists in several forms, including angiotensin I, II, III, and IV, each playing unique roles within the body. However, the focus primarily lies on angiotensin I and II due to their pivotal roles in the RAS and their significant physiological effects.
Focus on I and II
Angiotensin I and II are at the heart of the angiotensin discussion. Angiotensin I serves as a precursor, while angiotensin II is known for its active regulatory role in blood pressure and fluid balance.
Angiotensin I
Formation
Origin and Production
Angiotensin I originates from angiotensinogen, a protein produced by the liver. The conversion of angiotensinogen to angiotensin I is initiated by renin, an enzyme released by the kidneys in response to low blood pressure or decreased sodium chloride (NaCl) concentration in the blood.
Role of Renin
Renin’s role is pivotal as it marks the beginning of the renin-angiotensin system activation, leading to the production of angiotensin I. Renin’s release is a critical first step in the cascade that ultimately seeks to restore blood pressure and fluid balance.
Function
Precursor Role
Angiotensin I, on its own, has limited biological activity. Its primary function is serving as a precursor to angiotensin II. This conversion is a crucial step in the process that affects blood pressure and fluid regulation.
Limited Biological Activity
Despite its limited direct action, the role of angiotensin I is not to be underestimated. It is the necessary first step in the production of angiotensin II, which carries significant biological activity.
Angiotensin II
Creation
Conversion from Angiotensin I
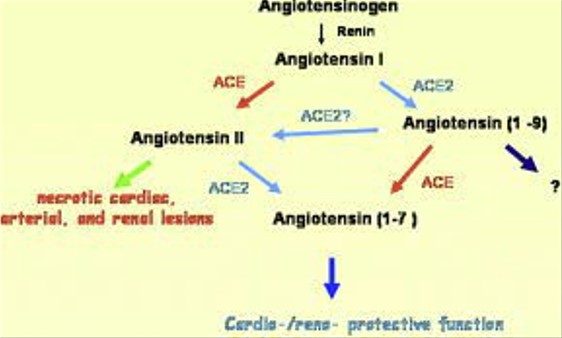
Angiotensin II is formed from angiotensin I through the action of angiotensin-converting enzyme (ACE), primarily in the lungs. This conversion is critical for activating angiotensin II’s physiological effects.
Enzymes Involved
The enzyme ACE is central to the conversion process. It transforms angiotensin I into angiotensin II by removing two of its amino acids, resulting in the octapeptide angiotensin II, the system’s active form.
Key Functions
Vasoconstriction
One of the primary actions of angiotensin II is vasoconstriction, the narrowing of blood vessels. This process increases blood pressure by reducing the diameter through which blood flows.
Aldosterone Secretion
Angiotensin II also stimulates the adrenal glands to secrete aldosterone, a hormone that increases sodium and water reabsorption in the kidneys. This action further raises blood pressure and adjusts the body’s fluid balance.
Impact on Blood Pressure and Fluid Balance
The combined effects of vasoconstriction and aldosterone secretion make angiotensin II a potent regulator of blood pressure and fluid balance. It ensures stability in the body’s internal environment, adjusting to meet physiological needs and maintaining cardiovascular health.
Comparative Analysis
Structural Differences
Amino Acid Sequence
Angiotensin I and II differ primarily in their amino acid sequence. Angiotensin I is a decapeptide, meaning it consists of 10 amino acids. On conversion to angiotensin II, it loses two amino acids, resulting in an octapeptide with 8 amino acids. This change in the sequence is crucial for the biological activity that angiotensin II exhibits.
Molecular Size
The molecular size of angiotensin also changes during this conversion. Angiotensin I, being a larger molecule due to its two extra amino acids, has a slightly higher molecular weight compared to angiotensin II. This reduction in size from angiotensin I to II is not just a numerical change but significantly impacts the molecules’ function and how they interact within the body.
Biological Impacts
Receptor Interaction
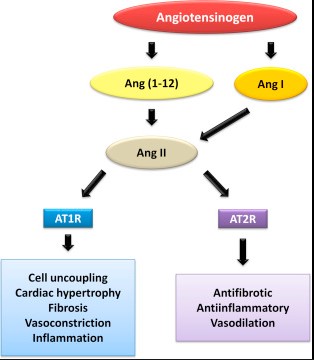
Angiotensin II’s ability to interact with receptors on the surface of cells is a defining feature of its role in the body. It binds to AT1 and AT2 receptors, with the interaction at AT1 receptors being responsible for most of the known actions of angiotensin II, including vasoconstriction, aldosterone secretion, and blood pressure regulation. Angiotensin I, due to its minimal direct activity, has limited interaction with these receptors.
Physiological Effects Comparison
The physiological effects of angiotensin I and II are markedly different due to their structural differences and receptor interactions. Angiotensin II, as a potent vasoconstrictor, directly increases blood pressure and influences fluid balance by stimulating aldosterone secretion. Angiotensin I, on the other hand, requires conversion to angiotensin II to exert significant physiological effects.
Role in Health and Disease
Contribution to Hypertension
Angiotensin II is a key contributor to hypertension. Its vasoconstrictive effects lead to increased blood pressure, and overactivity of the renin-angiotensin system can result in chronic hypertension. This condition is a major risk factor for cardiovascular disease, emphasizing the need to understand and modulate angiotensin II’s effects.
Involvement in Heart Failure
Heart failure is another condition where angiotensin II plays a significant role. In heart failure, the body often tries to compensate for reduced cardiac output by activating the renin-angiotensin system, which can exacerbate the condition by increasing blood pressure and workload on the heart. Managing angiotensin II’s effects is thus crucial in treating heart failure.
Therapeutic Aspects
Medications Targeting Angiotensin
ACE Inhibitors
ACE inhibitors are a class of medications that prevent the conversion of angiotensin I to angiotensin II by inhibiting the angiotensin-converting enzyme. This results in lower levels of angiotensin II, leading to vasodilation and decreased blood pressure. ACE inhibitors are widely used in the management of hypertension and heart failure.
Angiotensin II Receptor Blockers (ARBs)
Angiotensin II receptor blockers (ARBs) directly block the interaction of angiotensin II with AT1 receptors. This prevents the usual actions of angiotensin II, leading to vasodilation and reduced blood pressure. ARBs are another important tool in treating hypertension and heart failure, offering an alternative for patients who cannot tolerate ACE inhibitors.
Clinical Implications
Treatment of Hypertension
The treatment of hypertension often involves managing angiotensin II levels in the body. Both ACE inhibitors and ARBs are effective in lowering blood pressure by modulating the effects of angiotensin II. These medications not only reduce the risk of developing complications associated with hypertension but also improve overall cardiovascular health.
Management of Cardiac Conditions
In managing cardiac conditions such as heart failure, controlling angiotensin II’s effects is crucial. By reducing the workload on the heart and preventing excessive vasoconstriction, medications targeting the renin-angiotensin system can significantly improve patient outcomes. The choice between ACE inhibitors and ARBs often depends on patient tolerance and the specific needs of their condition, highlighting the personalized nature of cardiac care.
FAQs
What is Angiotensin?
Angiotensin is a peptide hormone critical for controlling blood pressure and the balance of fluids and salts in the body. It exists in multiple forms, but angiotensin I and II are the most significant, with the latter being particularly influential in regulating cardiovascular functions through vasoconstriction and aldosterone secretion.
How does Angiotensin I convert to Angiotensin II?
Angiotensin I is converted into angiotensin II by the angiotensin-converting enzyme (ACE), primarily in the lungs. This conversion is a key step in the renin-angiotensin system, leading to the active form that significantly affects blood pressure and fluid balance.
What are the main functions of Angiotensin II?
Angiotensin II is a powerful vasopressor that narrows blood vessels (vasoconstriction) and stimulates the production of aldosterone from the adrenal glands. These actions increase blood pressure and help the body adjust fluid and salt balances, which are vital for maintaining cardiovascular health and responding to physiological needs.
Why is Angiotensin important in medical treatment?
Angiotensin plays a pivotal role in the development and treatment of hypertension and heart failure. Medications targeting the renin-angiotensin system, such as ACE inhibitors and angiotensin II receptor blockers (ARBs), are foundational treatments for these conditions, highlighting the hormone’s significance in clinical medicine.
Conclusion
The distinction between angiotensin I and II underscores the complexity and sophistication of the body’s mechanisms for maintaining blood pressure and fluid equilibrium. Understanding these differences not only sheds light on the intricate workings of the cardiovascular system but also underscores the importance of targeted medical interventions in managing conditions like hypertension and heart failure. This knowledge forms the basis for developing effective treatments and advancing our capacity to manage and mitigate cardiovascular diseases.
In conclusion, the exploration of angiotensin I and II’s roles reveals the critical balance and interplay necessary for cardiovascular health. The continued research and development in this area promise further advancements in medical science, offering hope for improved outcomes in patients with cardiovascular diseases. The depth of our understanding directly influences the effectiveness of therapeutic strategies, making the study of angiotensin a key pillar in the pursuit of health and wellbeing.