The respiratory system plays a pivotal role in our survival, facilitating the exchange of oxygen and carbon dioxide between our bodies and the environment. Within this complex system lies the concept of dead space, areas where air does not contribute to gas exchange. Understanding the difference between anatomical and physiological dead space sheds light on the efficiency of breathing and the impact of various respiratory conditions.
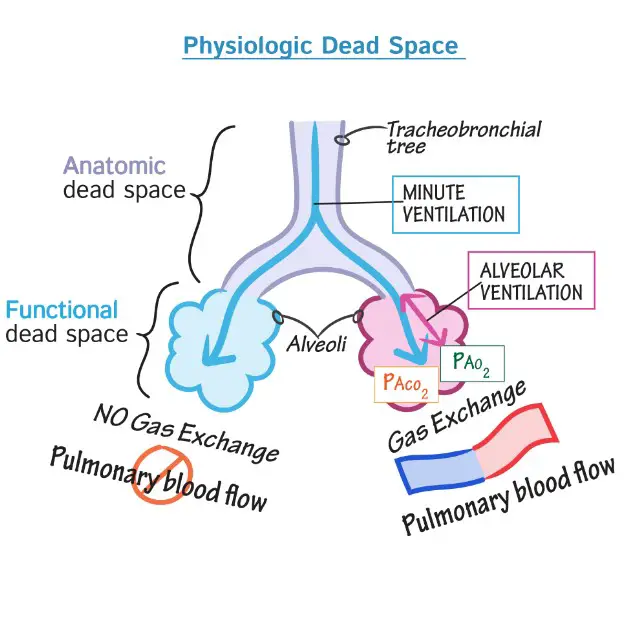
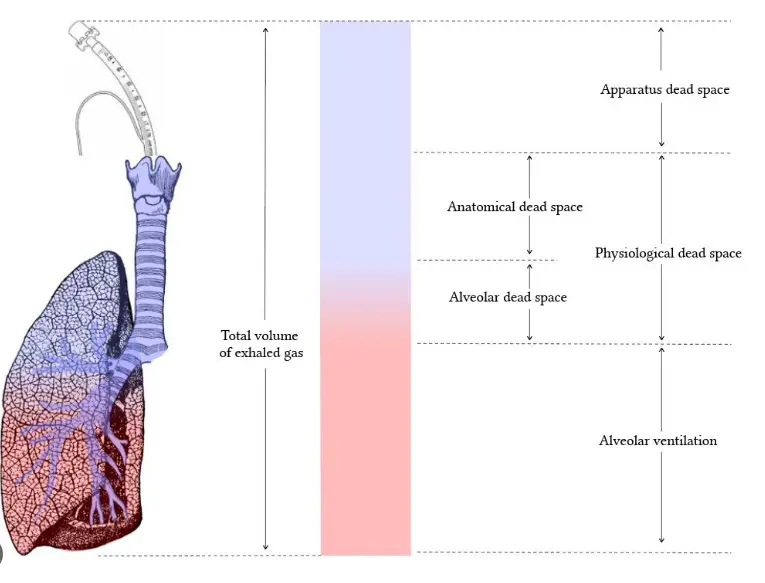
Anatomical dead space refers to the portions of the airways—such as the nose, pharynx, larynx, trachea, and bronchi—where no gas exchange occurs because they only transport air to the regions where exchange is possible. In contrast, physiological dead space includes the anatomical dead space plus any areas of the lungs where gas exchange is impaired or non-functional, even in the alveoli, due to issues like blood flow limitations or ventilation problems.
These concepts are not just academic; they have practical implications for respiratory health, affecting everything from the efficiency of oxygen delivery to the body’s tissues, to the management and prognosis of respiratory diseases. As we explore these differences further, we uncover the critical role dead space plays in our understanding of respiratory physiology and pathology, providing insights into the mechanisms behind healthy breathing and the challenges faced during respiratory illness.
Anatomical Dead Space
Definition
Anatomical dead space is a term used in respiratory physiology to describe parts of the airways where air travels but no gas exchange occurs. Essentially, it’s the volume of the breathing passages that only serves to move air to the alveoli, the tiny sacs where oxygen and carbon dioxide are exchanged with the bloodstream.
Components
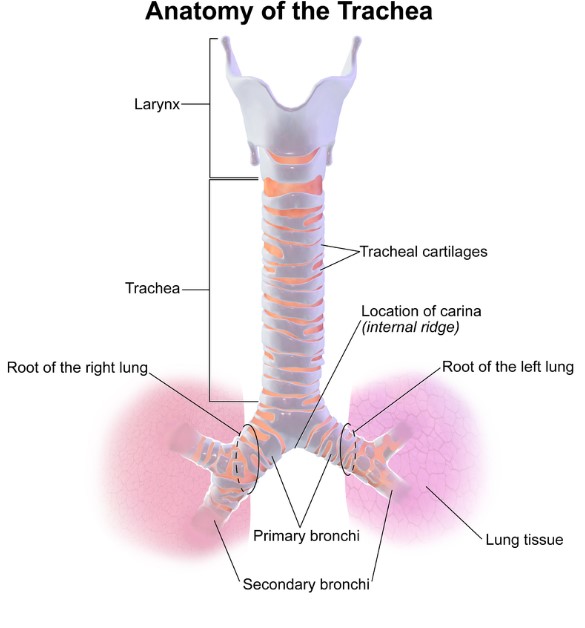
The respiratory tract is ingeniously designed, with its upper parts classified as anatomical dead space. These include:
- Nose: The primary entry point for inhaled air, playing a crucial role in air filtration.
- Pharynx and Larynx: Serve as passageways for air to move from the nose and mouth into the trachea.
- Trachea: Often referred to as the windpipe, it bifurcates into the two main bronchi.
- Bronchi: These are the large air passages that branch off the trachea and lead into the lungs.
Each of these components has a distinct function, but none participate directly in the gas exchange process. Instead, they act as conduits, delivering air to the lower respiratory tract where the alveoli are located.
Significance
While it might seem inefficient to have parts of the respiratory system that do not contribute to gas exchange, the anatomical dead space plays several vital roles:
- Warming and Humidifying Air: The air we breathe is adjusted to body temperature and saturated with water vapor, making gas exchange more efficient.
- Filtering: The nasal passages and trachea filter out particles and pathogens, protecting the delicate alveoli from damage or infection.
Physiological Dead Space
Definition
Physiological dead space takes the concept of dead space further, encompassing not only the anatomical dead space but also any regions in the lungs where gas exchange is impaired or non-functional. This includes areas where alveoli may be damaged, airflow is restricted, or blood flow to the alveoli is compromised.
Factors Influencing Increase
Several factors can lead to an increase in physiological dead space, often associated with lung disease or injury. These include:
- Pulmonary Embolism: A blockage in one of the pulmonary arteries reduces blood flow to parts of the lung, affecting gas exchange.
- Chronic Obstructive Pulmonary Disease (COPD): Characterized by airflow obstruction, reducing the effectiveness of gas exchange.
- Acute Respiratory Distress Syndrome (ARDS): A severe condition causing fluid to leak into the alveoli, diminishing their ability to exchange gases.
These conditions can significantly impact lung function, increasing the volume of physiological dead space and making breathing more laborious and less efficient.
Measurement
Understanding the extent of physiological dead space can be crucial in diagnosing and managing respiratory conditions. One common method for measuring this space is the Bohr equation, which calculates the difference between the total volume of expired air and the volume of air that has effectively participated in gas exchange. This method is invaluable in clinical settings, providing insights into the health of a patient’s lungs and guiding treatment decisions.
Comparing Dead Spaces
Key Differences
The distinction between anatomical and physiological dead spaces, while seemingly subtle, has profound implications for gas exchange and lung functionality. Anatomical dead space is fixed, comprising parts of the respiratory system that merely transport air to the gas exchange sites without participating in the exchange itself. In contrast, physiological dead space is variable, encompassing both the anatomical dead space and any additional areas where gas exchange is compromised due to various pathologies or conditions.
The primary differences include:
- Functionality: Anatomical dead space serves as an air conduit, while physiological dead space includes areas of compromised gas exchange.
- Variability: Anatomical dead space is relatively constant, whereas physiological dead space can increase with lung conditions.
- Measurement: The measurement of physiological dead space, incorporating the Bohr equation, reflects lung health more comprehensively than the static concept of anatomical dead space.
Clinical Relevance
In clinical settings, distinguishing between these types of dead space aids in diagnosing and managing respiratory conditions. An increase in physiological dead space often signals underlying lung pathology that requires specific interventions. This differentiation is crucial for:
- Diagnosis: Elevated physiological dead space may indicate conditions such as COPD, pulmonary embolism, or ARDS.
- Treatment Planning: Understanding the extent of physiological dead space helps tailor treatment strategies, such as ventilator settings in critically ill patients.
- Prognosis Evaluation: Increased physiological dead space can be a predictor of outcomes in patients with acute respiratory distress syndrome or undergoing major surgery.
Impacts on Health
Respiratory Efficiency
Variations in dead space directly influence respiratory efficiency. A balance between ventilation and perfusion is essential for optimal gas exchange; an imbalance, manifested as increased dead space, leads to decreased oxygenation of blood and increased carbon dioxide levels. Factors affecting this balance include:
- Alveolar Ventilation: Adequate ventilation of the alveoli is necessary for efficient gas exchange. Increased dead space reduces the fraction of inhaled air that reaches these gas exchange sites.
- Blood Perfusion: Conditions that impair blood flow to the alveoli further complicate the ventilation-perfusion mismatch, exacerbating the inefficiency.
Disease and Dysfunction
Chronic Obstructive Pulmonary Disease (COPD), Pulmonary Embolism, and Acute Respiratory Distress Syndrome (ARDS) are prime examples of conditions that can significantly increase physiological dead space. Each of these diseases affects the lung’s architecture or blood flow, leading to:
- Reduced Gas Exchange: The inability to adequately exchange gases results in hypoxemia and hypercapnia, manifesting as shortness of breath and increased work of breathing.
- Complications: An increase in dead space can lead to complications, including respiratory failure and the need for mechanical ventilation.
Monitoring and Management
Evaluating dead space is a key component in the monitoring and management of patients with respiratory issues. Strategies focusing on minimizing physiological dead space are essential, especially in critically ill patients or those with chronic respiratory diseases. These include:
- Ventilation Strategies: Adjusting ventilator settings to improve alveolar ventilation without causing lung injury.
- Treating Underlying Causes: Addressing the primary cause of increased physiological dead space, such as anticoagulation for pulmonary embolism.
- Monitoring Progress: Regular assessment of physiological dead space can help gauge the effectiveness of treatments and adjust them as necessary.

FAQs
What is Anatomical Dead Space?
Anatomical dead space consists of the airways that transport air to the alveoli but do not participate in the gas exchange process themselves. This includes structures like the trachea and bronchi, which are essential for moving air but do not directly contribute to oxygen entering the bloodstream or carbon dioxide being expelled.
How is Physiological Dead Space Measured?
Physiological dead space is typically measured using the Bohr equation, which calculates the difference between the total volume of expired air and the volume of air that has participated in gas exchange. This measurement is crucial for assessing lung efficiency and diagnosing respiratory conditions.
Why Does Dead Space Matter in Respiratory Health?
Dead space matters in respiratory health because it influences the efficiency of gas exchange in the lungs. An increase in dead space can lead to reduced oxygen delivery to the body and increased effort in breathing, which can exacerbate or indicate underlying respiratory conditions.
Can Dead Space Increase with Lung Disease?
Yes, dead space can increase with lung disease. Conditions such as chronic obstructive pulmonary disease (COPD), pulmonary embolism, and acute respiratory distress syndrome (ARDS) can all increase physiological dead space by impairing gas exchange or reducing blood flow to the alveoli.
Conclusion
Distinguishing between anatomical and physiological dead space is more than an academic exercise; it is a fundamental aspect of understanding respiratory health and disease. These concepts help medical professionals diagnose and manage respiratory conditions more effectively, highlighting the importance of efficient gas exchange and the impact of dead space on respiratory function.
In conclusion, the exploration of dead space in the respiratory system reveals the intricacies of how we breathe and the challenges faced by those with respiratory conditions. By understanding these differences, we can appreciate the delicate balance required for effective gas exchange and the significance of maintaining respiratory health for overall well-being.