Thrombolytic therapy has revolutionized the treatment of acute ischemic stroke and myocardial infarction by dissolving blood clots that block blood flow to critical areas of the body. Among the agents used, alteplase and tenecteplase stand out as key players in this field. Their roles, while distinct, overlap in their purpose to save lives and reduce long-term disability in patients suffering from these conditions.
Alteplase and tenecteplase are both tissue plasminogen activators used in the treatment of stroke and heart attacks, but they differ in their molecular structure, clinical applications, and dosing regimens. Alteplase, often administered soon after the onset of symptoms, requires a complex dosing schedule. In contrast, tenecteplase offers a simpler, single-dose administration, making it a preferred choice in specific scenarios for its ease of use and quick administration.
Understanding the nuances between alteplase and tenecteplase is crucial for medical professionals as they navigate treatment options. The choice between these two agents can significantly impact patient outcomes, influenced by factors such as the time since symptom onset, the type of medical emergency, and the patient’s overall health profile.
Alteplase Overview
What Is Alteplase?
Alteplase is a thrombolytic or clot-busting medication, widely recognized under the brand name Activase. Its primary function is to dissolve dangerous blood clots in blood vessels, which can lead to serious medical conditions like stroke and heart attacks. As a tissue plasminogen activator (tPA), alteplase plays a crucial role in emergency medical interventions.
Clinical Uses
Alteplase is predominantly used in the treatment of:
- Acute ischemic stroke: Administered within a narrow time window, ideally within 3 to 4.5 hours from the onset of symptoms.
- Acute myocardial infarction (AMI) or heart attack: It helps to restore blood flow to the heart.
- Acute massive pulmonary embolism: Though less common, it’s used to address blood clots in the lungs.
The aim is to swiftly dissolve clots, restore blood flow, minimize damage to the affected tissues, and ultimately, save lives and reduce long-term disabilities.
Mechanism of Action
Alteplase works by converting plasminogen, a natural substance in the body, into plasmin. Plasmin then breaks down the fibrin framework of blood clots, effectively dissolving them. This action restores normal blood flow and prevents the potential damage caused by prolonged blockages.
Dosage and Administration
The administration of alteplase must be precise, and it varies depending on the condition being treated:
- Stroke: The standard dose is 0.9 mg/kg (not exceeding 90 mg total), with 10% of the total dose administered as an initial intravenous (IV) bolus over 1 minute, followed by the remaining dose over 60 minutes.
- AMI: Dosage can differ but typically involves a larger bolus dose followed by a continuous infusion.
- Pulmonary Embolism: Similar to the AMI treatment, with specific dosages based on body weight.
Timely administration is critical for effectiveness, particularly in stroke patients.
Side Effects and Risks
While alteplase can be life-saving, it’s not without risks. The most significant is the risk of bleeding, including:
- Intracranial hemorrhage: A rare but serious side effect, particularly in stroke patients.
- Gastrointestinal bleeding
- Bleeding at the injection site
Patients must be carefully selected and monitored for any signs of bleeding during and after alteplase administration.
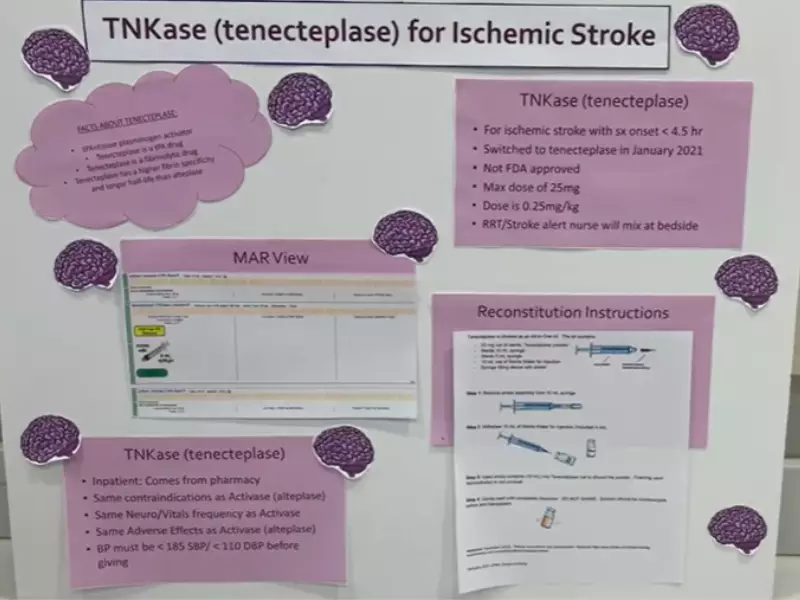
Tenecteplase Overview
What Is Tenecteplase?
Tenecteplase, sold under the brand name TNKase, is another thrombolytic drug similar to alteplase but with a few key differences. It’s engineered to have a longer half-life and greater fibrin specificity, which allows for a single, rapid administration. This makes tenecteplase a preferred option in certain scenarios, particularly in treating acute myocardial infarction.
Clinical Uses
Tenecteplase is primarily used for:
- Acute myocardial infarction: Its quick, single-dose administration is highly beneficial in emergency settings.
- Ischemic stroke: While less common, some studies suggest tenecteplase may be effective and possibly preferable due to its ease of administration.
Its role in treating pulmonary embolism is still under investigation.
Mechanism of Action
Like alteplase, tenecteplase works by converting plasminogen to plasmin. However, its modified structure increases its affinity for fibrin and resistance to plasminogen activator inhibitor-1 (PAI-1). This enhances its clot-busting ability and allows for the simpler dosing regimen.
Dosage and Administration
The defining feature of tenecteplase is its single-dose administration, which varies based on the patient’s weight, particularly for heart attack treatment. This simplifies the emergency treatment process significantly, allowing for faster intervention.
Side Effects and Risks
The risks associated with tenecteplase are similar to those of alteplase, with bleeding being the primary concern. However, its specific side effect profile can slightly differ due to its molecular structure and the conditions it treats. As with alteplase, careful patient selection and monitoring are crucial to minimize these risks.
Comparison and Conclusion
Both alteplase and tenecteplase are pivotal in the treatment of acute cardiovascular and cerebrovascular events. Their differences in dosing and molecular design offer options to healthcare providers, tailoring treatment strategies to individual patient needs. Understanding these thrombolytics’ mechanisms, applications, and safety profiles is essential for maximizing their benefits while mitigating risks.
Comparative Analysis
Key Similarities
Alteplase and tenecteplase share several important features, primarily their role as thrombolytic agents used in urgent medical situations. Both drugs are forms of tissue plasminogen activator (tPA), designed to dissolve blood clots by converting plasminogen to plasmin. Their use in treating acute ischemic stroke and myocardial infarction highlights their critical place in emergency medicine, aiming to restore blood flow and minimize tissue damage swiftly.
Key Differences
Despite their similar applications, alteplase and tenecteplase differ significantly in their molecular structure, leading to variations in their pharmacokinetics and administration protocols. Tenecteplase is a genetically modified form of tPA with a longer half-life and increased fibrin specificity, which allows for a single-dose administration. In contrast, alteplase requires a more complex dosing regimen, often involving an initial bolus followed by an infusion over several hours.
Efficacy
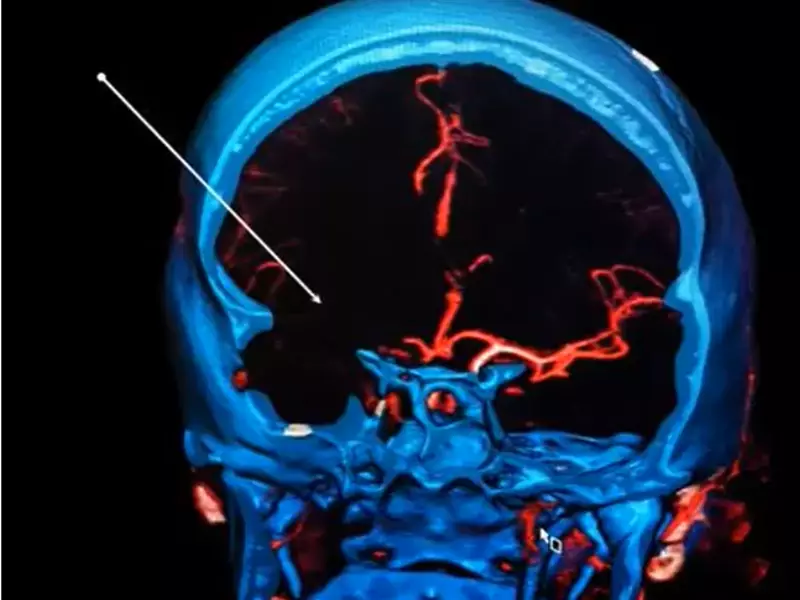
Comparison in Stroke Treatment
In treating acute ischemic stroke, both alteplase and tenecteplase have shown effectiveness. However, studies suggest that tenecteplase might offer comparable or even superior outcomes in certain patient populations due to its ease of administration and potential for quicker reperfusion. The decision between the two often depends on the time since symptom onset and specific patient factors.
Comparison in Myocardial Infarction
For myocardial infarction, tenecteplase’s single-dose regimen provides a distinct advantage, especially in settings where rapid treatment initiation is crucial. Its efficacy in quickly dissolving clots in the coronary arteries has made it a preferred choice in many emergency departments. Alteplase, while effective, is more commonly used when tenecteplase is not available or when specific patient conditions warrant its use.
Safety Profile
Side Effect Comparison
Both medications carry the risk of bleeding, the most significant side effect of thrombolytic therapy. However, the incidence and severity of bleeding complications can vary between the two, with some studies suggesting a lower risk associated with tenecteplase in certain contexts.
Risk of Bleeding
The risk of bleeding, particularly intracranial hemorrhage, necessitates careful patient selection and monitoring. Factors such as age, the severity of the stroke, and prior medical history must be considered to minimize this risk. While both drugs require stringent monitoring, the single-dose nature of tenecteplase simplifies its administration process, potentially reducing the time frame for monitoring acute side effects.
Administration
Dosage Differences
The dosage of alteplase is typically 0.9 mg/kg (up to a maximum of 90 mg), with part given as an initial bolus and the remainder infused over an hour. Tenecteplase dosage is weight-based, administered in a single bolus, which streamlines its use in emergency scenarios.
Administration Convenience
The simplicity of tenecteplase’s single-dose administration offers a clear advantage in emergency settings, allowing for faster treatment initiation. This can be particularly beneficial in rural or underserved areas where medical resources are limited.
Clinical Considerations
Patient Selection Criteria
Selecting the right thrombolytic agent requires consideration of several factors, including:
- Time since symptom onset: Alteplase is generally considered if treatment can be initiated within 4.5 hours for stroke patients.
- Patient’s overall health: Pre-existing conditions and contraindications can influence the choice between alteplase and tenecteplase.
- Type of medical emergency: The specific nature of the clot-related emergency can guide the selection process.
Cost Considerations
The cost of treatment is an important consideration, with alteplase generally being more expensive due to its complex administration. However, the overall cost must also account for the potential need for extended hospital stays and monitoring, where tenecteplase may offer cost savings through its simplified administration.
Accessibility and Availability
Accessibility to these medications can vary globally, with alteplase being more widely available in some regions. However, tenecteplase’s ease of use and storage may increase its accessibility in remote or resource-limited settings, offering a viable option where rapid treatment is needed.
Frequently Asked Questions
What is thrombolytic therapy?
Thrombolytic therapy is a medical treatment used to dissolve blood clots that have formed in the blood vessels, restoring normal blood flow and preventing damage to tissues and organs. This therapy is critical in treating conditions such as acute ischemic stroke and myocardial infarction, where timely intervention can save lives and reduce long-term disabilities.
How do alteplase and tenecteplase work?
Alteplase and tenecteplase are types of tissue plasminogen activators. They work by converting plasminogen to plasmin, an enzyme that breaks down clots. While both serve the same purpose, their differences lie in their molecular structure and pharmacokinetics, affecting their dosage and administration protocols.
When are alteplase and tenecteplase used?
Alteplase and tenecteplase are used in the emergency treatment of acute ischemic stroke, myocardial infarction, and, less commonly, for the treatment of acute massive pulmonary embolism. The choice between them depends on the specific circumstances of the patient’s condition, including timing, severity, and individual health factors.
What are the main differences between alteplase and tenecteplase?
The main differences between alteplase and tenecteplase include their dosing schedules and molecular structures. Alteplase requires a more complex administration protocol, while tenecteplase can be administered in a single dose. Additionally, tenecteplase has a modified structure that offers greater fibrin specificity and resistance to plasminogen activator inhibitor-1, potentially offering advantages in certain situations.
Conclusion
Alteplase and tenecteplase play indispensable roles in the treatment of life-threatening conditions such as stroke and heart attacks. Their effective use requires a deep understanding of their pharmacological differences and clinical applications. Choosing the right agent can be pivotal in achieving the best possible outcomes for patients, making the knowledge of these differences essential for healthcare professionals.
The advancements in thrombolytic therapy exemplify the progress in medical science, providing us with powerful tools to combat previously insurmountable conditions. As research continues and our understanding deepens, the potential to refine these treatments and improve patient care is vast, promising a future where the impact of acute vascular events can be minimized further.
