Hemolysis, the breakdown of red blood cells, serves as a crucial diagnostic indicator in microbiology, particularly in identifying pathogenic bacteria. When cultured on specific agar plates, the reaction of bacteria with blood cells results in distinct patterns of hemolysis: alpha, beta, and gamma. Each type provides essential clues about the bacterial species present.
Alpha, beta, and gamma hemolysis are differentiated by their effects on blood cells. Alpha hemolysis partially breaks down hemoglobin, causing a greenish discoloration on the agar. Beta hemolysis completely lyses red blood cells, resulting in a clear zone around bacterial colonies. Gamma hemolysis shows no change or lysis of red blood cells, leaving the agar unchanged.
In medical diagnostics, recognizing these hemolysis patterns helps clinicians understand the type of bacterial infection present, guiding treatment decisions. The ability to distinguish between these types is particularly significant in cases of streptococcal infections, where treatment protocols vary dramatically based on the type of hemolysis exhibited.
Hemolysis Explained
What is Hemolysis?
Hemolysis refers to the breakdown or destruction of red blood cells (RBCs). This process occurs when the cell membrane of red blood cells ruptures, releasing hemoglobin into the surrounding fluid. In a medical or microbiological context, hemolysis is often observed when blood cells are exposed to certain bacterial enzymes or toxins. The study of hemolysis is pivotal in the field of microbiology as it aids in the identification of various bacterial species based on their hemolytic properties.
Role in Bacterial Identification
In clinical diagnostics, observing how bacteria interact with red blood cells on nutrient-rich media, such as blood agar, provides essential clues about their identity and potential pathogenicity. Bacteria that cause hemolysis exhibit specific patterns that are crucial for their identification and the subsequent selection of appropriate treatment strategies.
Types of Hemolysis
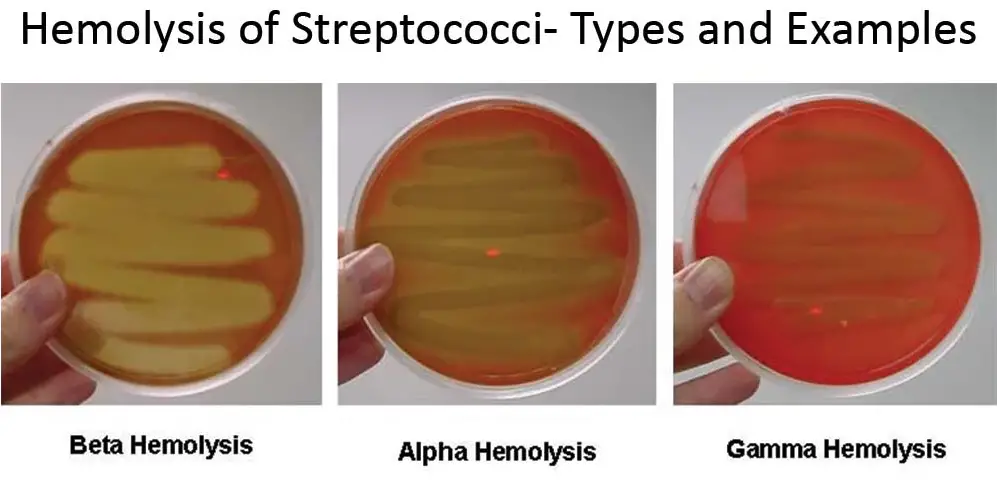
There are three main types of hemolysis: alpha, beta, and gamma. Each type is distinguished by a different visual effect on blood agar, which is used to cultivate the bacteria.
Overview of the Three Types
- Alpha Hemolysis: Partial hemolysis that results in a greenish or dark discoloration on the agar.
- Beta Hemolysis: Complete lysis of red blood cells, appearing as a clear zone surrounding the bacteria.
- Gamma Hemolysis: No hemolysis or change in the blood agar around the bacteria.
Significance in Clinical Settings
The type of hemolysis exhibited by bacteria is not just a diagnostic feature; it often correlates with the virulence of the organism. Identifying whether a bacterium is alpha, beta, or gamma-hemolytic helps clinicians determine the potential severity of infection and guides antibiotic treatment decisions.
Alpha Hemolysis
Characteristics of Alpha Hemolysis
Alpha hemolysis, also known as partial hemolysis, is characterized by the reduction of hemoglobin to methemoglobin in the red blood cells, which imparts a greenish color to the agar. This change is due to the bacterial production of hydrogen peroxide which oxidizes the hemoglobin.
Visual Appearance on Agar
On blood agar plates, alpha-hemolytic bacteria produce a zone of green, brown, or olive discoloration around the colonies. This is a crucial visual cue in microbiology labs for identifying certain bacterial strains.
Mechanism of Hemolysis
The mechanism involves the partial degradation of red blood cell walls by enzymes such as peroxidases, produced by the bacteria. These enzymes modify hemoglobin, leading to the characteristic color change.
Common Bacteria
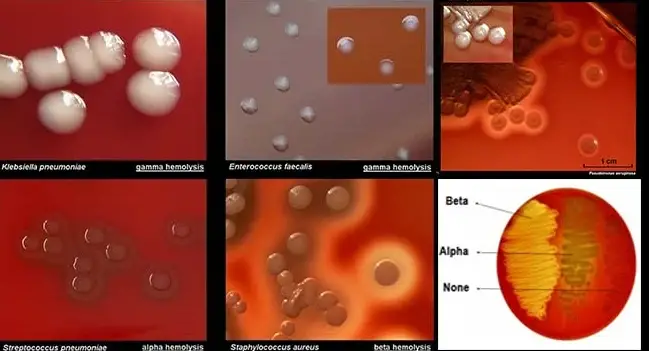
Common alpha-hemolytic bacteria include Streptococcus pneumoniae and Streptococcus viridans. These organisms are often associated with conditions like dental caries, meningitis, and respiratory infections.
Associated Diseases and Conditions
- Streptococcus pneumoniae: Pneumonia, meningitis, and bloodstream infections.
- Streptococcus viridans: Endocarditis, especially in people with underlying heart conditions.
Beta Hemolysis
Characteristics of Beta Hemolysis
Beta hemolysis represents a complete destruction of red blood cells, leading to a clear zone surrounding the bacterial colonies on blood agar. This type of hemolysis is more aggressive and is often associated with more pathogenic bacteria.
Visual Appearance on Agar
The clear zone in beta hemolysis indicates that the hemoglobin in the red blood cells has been completely lysed. This stark clearing is often used as a definitive test for the presence of certain bacterial species.
Mechanism of Hemolysis
Beta-hemolytic bacteria produce enzymes such as streptolysin, which completely lyse red blood cells. The enzymes break down the cell membrane, allowing the bacteria to access nutrients within the red blood cells.
Common Bacteria
Beta-hemolytic bacteria include Streptococcus pyogenes and Staphylococcus aureus. These bacteria are capable of causing severe diseases.
Associated Diseases and Conditions
- Streptococcus pyogenes: Strep throat, scarlet fever, and rheumatic fever.
- Staphylococcus aureus: Skin infections, pneumonia, and toxic shock syndrome.
Gamma Hemolysis
Characteristics of Gamma Hemolysis
Gamma hemolysis, or more accurately non-hemolysis, is characterized by the absence of red blood cell destruction. This type of reaction results in no visible change to the blood agar around the colonies of bacteria. This non-hemolytic behavior is significant because it differentiates certain benign or less aggressive bacteria from those causing clear or partial hemolysis.
Explanation of Non-hemolytic Reaction
In gamma hemolysis, the bacteria do not produce hemolysins, the enzymes responsible for breaking down red blood cells. Therefore, the blood agar remains unchanged, maintaining its original color and clarity, indicating that the red cells are intact.
Visual Identification
Identifying gamma hemolysis involves observing a lack of discoloration or clearing around bacterial colonies on a blood agar plate. The agar around the colonies will look exactly as it did before incubation, without any of the tell-tale signs of alpha or beta hemolysis.
Common Bacteria
Examples of gamma-hemolytic bacteria include Enterococcus faecalis and certain strains of Staphylococcus epidermidis. These bacteria are often part of the normal flora of the human body and are less frequently associated with severe infections.
Clinical Relevance
Although gamma hemolysis indicates non-lytic behavior, the presence of these bacteria can still be clinically relevant, especially in immunocompromised individuals or in hospital settings where opportunistic infections are a concern.
Comparative Analysis
Alpha vs Beta Hemolysis
The key differences between alpha and beta hemolysis lie in the degree of hemoglobin breakdown and the bacterial enzymes involved. Alpha hemolysis partially degrades hemoglobin, leading to a greenish discoloration, while beta hemolysis completely clears red blood cells, resulting in a transparent halo around colonies. Clinically, beta-hemolytic bacteria are often more aggressive, necessitating prompt and effective treatment to prevent severe outcomes.
Beta vs Gamma Hemolysis
Beta and gamma hemolysis are at opposite ends of the hemolytic spectrum. Beta hemolysis indicates a high level of aggressiveness and pathogenic potential, often requiring aggressive therapeutic measures. In contrast, gamma hemolysis suggests a non-lytic and typically less harmful bacterial presence, which might not always require treatment unless it’s an opportunistic infection in vulnerable patients.
Alpha vs Gamma Hemolysis
Alpha and gamma hemolysis can sometimes be confused due to the subtle nature of alpha hemolysis’ discoloration. However, alpha-hemolytic bacteria are active in altering hemoglobin, albeit partially, which can still play a role in infections such as pneumonia or meningitis. Gamma-hemolytic bacteria, on the other hand, do not alter the red blood cells at all, which generally indicates a lower risk of serious disease.
Diagnostic Techniques
Culturing Methods
To detect hemolysis in the laboratory, microbiologists use blood agar plates:
- Preparation: A nutrient-rich base with a high concentration of sheep or horse blood.
- Incubation: Bacteria are cultured on these plates and incubated at body temperature to mimic human conditions.
Agar Types Used
- Sheep Blood Agar: Most commonly used for detecting hemolytic activity.
- Horse Blood Agar: Used for certain types of bacteria which show enhanced hemolytic properties on this medium.
Clinical Applications
Role in Diagnosing Infections
The type of hemolysis observed plays a crucial role in diagnosing bacterial infections. Alpha and beta hemolysis often indicate pathogenic bacteria that might require specific antibiotic treatments.
Decision-making Based on Hemolysis Type
The detection of hemolysis type helps clinicians determine the urgency and type of treatment:
- Beta Hemolysis: Typically requires immediate and aggressive treatment.
- Alpha and Gamma Hemolysis: Treatment varies based on the bacteria identified and the patient’s overall health condition.
Case Studies
Real-world Examples
Instances where hemolysis identification directly influenced patient outcomes include:
- Streptococcus pyogenes infections: Rapid identification and treatment based on beta hemolysis detection have been critical in preventing complications like rheumatic fever.
- Identification of harmless flora: Gamma hemolysis helped confirm the non-pathogenic nature of certain bacteria, avoiding unnecessary treatments.
Outcomes and Lessons Learned
These cases underline the importance of accurate hemolysis detection in clinical microbiology. They demonstrate the critical link between laboratory diagnostics and effective patient care, emphasizing how fundamental microbial growth observations are in guiding clinical decisions.
Frequently Asked Questions
What causes hemolysis?
Hemolysis is primarily caused by the enzymes produced by bacteria that either completely or partially destroy red blood cells. In a clinical lab setting, this enzymatic activity is observed when bacteria are cultured on blood agar plates.
Why is beta hemolysis considered more severe?
Beta hemolysis indicates a complete breakdown of red blood cells, often associated with more aggressive bacterial infections. This type of hemolysis is typically caused by bacteria like Streptococcus pyogenes, known for severe infections such as strep throat or rheumatic fever.
How is alpha hemolysis identified?
Alpha hemolysis is identified by a green or brown discoloration around the bacterial colony on blood agar. This discoloration results from the partial oxidation of hemoglobin to methemoglobin in the red blood cells.
Can gamma hemolysis indicate an infection?
Gamma hemolysis, or non-hemolysis, indicates that the bacteria do not lyse red blood cells. While this may suggest a less aggressive bacterial strain, it does not necessarily mean there is no infection. Some pathogens exhibit gamma hemolysis and still cause infections.
What is the role of blood agar in diagnosing infections?
Blood agar plays a crucial role in diagnosing infections as it helps to identify and differentiate bacteria based on their hemolytic properties. The type of hemolysis exhibited can guide clinicians in determining the nature of the bacterial pathogen involved.
Conclusion
The differentiation between alpha, beta, and gamma hemolysis is more than a simple laboratory observation; it is a critical component in diagnosing bacterial infections. Recognizing these patterns allows healthcare providers to administer the most effective treatments based on the specific type of bacterial invasion.
In sum, the ability to accurately interpret hemolysis results is indispensable in clinical microbiology. This knowledge not only aids in the immediate treatment of bacterial infections but also enhances our broader understanding of microbial pathogens and their interactions with the human host.

