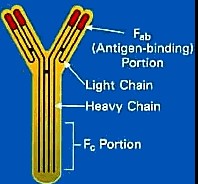
Antibodies are crucial components of the immune system, guarding against infections and diseases by recognizing and neutralizing foreign substances known as antigens. Among the vast array of antibodies, alloantibodies and autoantibodies stand out for their specific roles and implications in human health. These antibodies, though similar in their basic structure and function of antigen recognition, differ significantly in their origin and the way they impact the body.
Alloantibodies are formed in response to foreign antigens present in another individual of the same species, typically observed in situations like blood transfusions and organ transplants. Autoantibodies, on the other hand, are produced when the immune system mistakenly targets and reacts against the body’s own cells and tissues. This fundamental difference highlights the contrasting roles they play, with alloantibodies being central to transplant compatibility and autoantibodies being key factors in autoimmune diseases.
Understanding the distinction between alloantibodies and autoantibodies is not just academic; it has practical implications in clinical diagnosis, treatment of autoimmune diseases, and the management of transplant rejections. These antibodies exemplify the immune system’s complexity and its double-edged nature—protective in recognizing foreign threats but potentially harmful when misdirected against self-antigens.
Alloantibody Explained
Definition
Alloantibodies are antibodies produced by the immune system in response to antigens that come from another individual of the same species. Unlike the antibodies generated against common pathogens, alloantibodies target the genetic differences between individuals of the same species, such as those found in blood types or transplanted organs.
Formation Process
The process of alloantibody formation is triggered when the immune system encounters cells or tissues that have antigens different from those of the host. This can occur during:
- Blood transfusions, where blood from a donor has different surface antigens.
- Pregnancy, where fetal cells cross into the maternal circulation, exposing the mother to new antigens.
- Organ transplantation, where the transplanted organ carries antigens foreign to the recipient’s immune system.
Upon exposure, the immune system recognizes these foreign antigens and mounts a response, producing alloantibodies that specifically target the identified antigens.
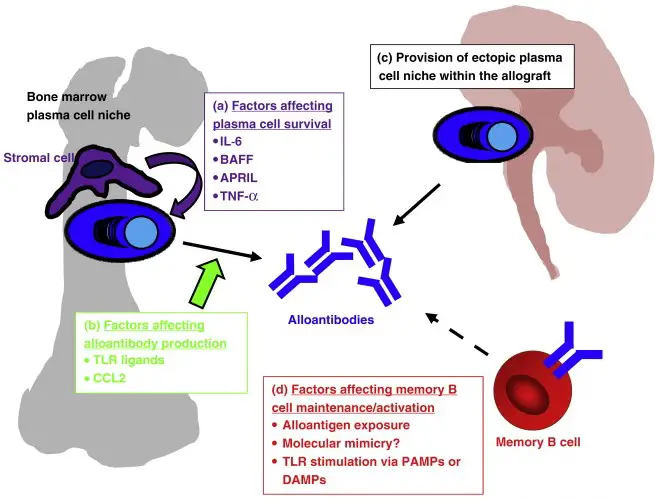
Role in Transplantation
In transplantation, alloantibodies can significantly impact the success and longevity of the graft. Their presence can lead to:
- Acute rejection: A rapid response against the transplanted organ, potentially leading to organ failure.
- Chronic rejection: Long-term damage to the transplant, resulting in a slow decline in function.
Preventing and managing alloantibody-mediated rejection involves:
- Matching donor and recipient: Reducing the antigenic difference between the donor and recipient to minimize the immune response.
- Immunosuppression: Using medications to suppress the immune response and reduce the production of harmful alloantibodies.
Examples in Clinical Settings
In clinical settings, alloantibodies are encountered in scenarios such as:
- Hemolytic Disease of the Newborn (HDN): Where maternal alloantibodies target fetal red blood cells.
- Transfusion reactions: Reactions occur when a recipient’s alloantibodies react against transfused blood.
Autoantibody Overview
Definition
Autoantibodies are antibodies that mistakenly target and react against an individual’s own cells and tissues. Unlike alloantibodies, which target differences between individuals, autoantibodies arise from a breakdown in the immune system’s ability to distinguish between self and non-self.
How They Form
Autoantibodies form due to a loss of tolerance, where the immune system fails to recognize certain self-antigens as harmless. Factors contributing to this loss of tolerance include:
- Genetic predisposition: Certain genes increase the risk of autoimmune responses.
- Environmental triggers: Infections, chemicals, or physical stress can initiate autoantibody production.
- Molecular mimicry: The immune system confuses self-antigens with similar foreign antigens.
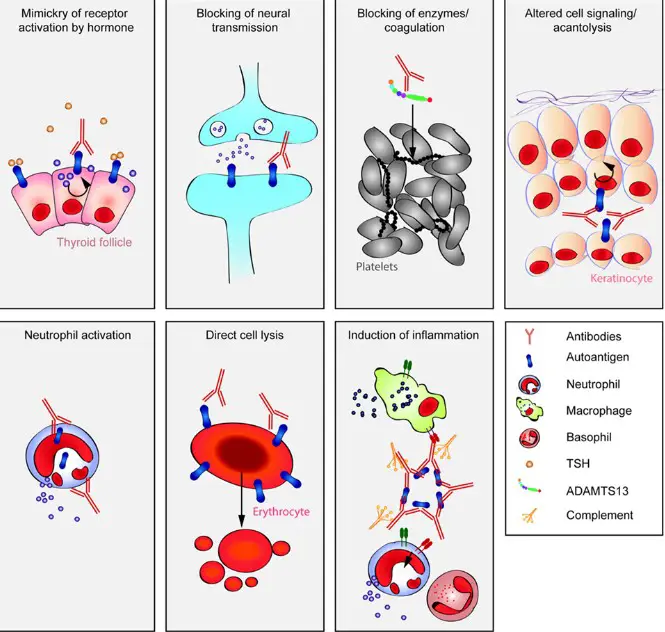
Impact on Health
The presence of autoantibodies can lead to autoimmune diseases, where the immune system’s attack on self-tissues causes inflammation, damage, and dysfunction. The impact varies based on the specific autoantibodies involved and the tissues targeted, ranging from localized symptoms to systemic disorders.
Common Autoimmune Diseases
Examples of autoimmune diseases include:
- Rheumatoid arthritis: Autoantibodies attack joints, causing pain and inflammation.
- Lupus: A systemic condition where autoantibodies target various organs.
- Type 1 diabetes: Autoantibodies destroy insulin-producing cells in the pancreas.
Key Differences
Origin
- Alloantibodies arise from exposure to foreign antigens from another individual of the same species.
- Autoantibodies result from the immune system attacking the body’s own cells.
Function
- Alloantibodies play a role in immune responses against perceived external threats from the same species, such as in blood transfusions or organ transplants.
- Autoantibodies are involved in autoimmune diseases, mistakenly targeting self-antigens.
Health Implications
- Alloantibodies can cause complications in blood transfusions, organ transplants, and pregnancies.
- Autoantibodies are markers and mediators of autoimmune diseases, leading to chronic conditions and systemic disorders.
Detection Methods
Detecting these antibodies involves different laboratory tests tailored to the specific antibodies and their associated conditions:
- For alloantibodies: Screening tests before transfusions or transplants to assess compatibility.
- For autoantibodies: Tests like ANA (antinuclear antibody) for lupus or RF (rheumatoid factor) for rheumatoid arthritis to aid in diagnosis.
Clinical Significance
In Transplant Rejection
The role of alloantibodies in transplant rejection is a critical area of concern in transplantation medicine. When alloantibodies recognize and bind to antigens on the transplanted organ, they can activate the immune system’s attack, leading to rejection. This phenomenon underlines the necessity of precise matching and immune management to ensure transplant success. Strategies to mitigate alloantibody-mediated rejection include:
- Immunosuppressive therapy: To reduce the immune system’s ability to produce alloantibodies.
- Desensitization protocols: To decrease the levels of pre-existing alloantibodies in recipients with high risk.
Autoimmune Disease Diagnosis
Diagnosing autoimmune diseases involves detecting autoantibodies that target specific self-antigens. The presence of certain autoantibodies can be indicative of specific autoimmune diseases, such as:
- Antinuclear antibodies (ANAs) for systemic lupus erythematosus (SLE),
- Rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs) for rheumatoid arthritis (RA).
Identifying these autoantibodies helps clinicians diagnose and monitor disease progression and response to treatment.
Treatment Strategies
Treatment strategies for conditions involving alloantibodies and autoantibodies must be tailored to the individual’s needs, focusing on managing symptoms, preventing organ damage, and maintaining quality of life. This includes immunosuppression, plasmapheresis to remove harmful antibodies, and the use of targeted biological therapies designed to modify the immune response.
Detection and Measurement
Laboratory Tests
The detection and measurement of alloantibodies and autoantibodies are primarily conducted through laboratory tests, including:
- Enzyme-linked immunosorbent assay (ELISA): For quantitative measurement of antibodies.
- Flow cytometry: To assess antibodies against specific cell surface antigens.
- Indirect immunofluorescence: For detecting a wide range of autoantibodies by visualizing their binding to cells or tissues.
These tests are vital for diagnosing autoimmune diseases, assessing transplant compatibility, and monitoring patients’ response to therapy.
Interpreting Results
Interpreting the results of antibody tests requires expertise, as the presence of specific antibodies can indicate different conditions based on their concentration, the clinical context, and the presence of other antibodies. A positive result may necessitate further testing or immediate clinical intervention, depending on the condition being investigated.
Advancements in Technology
Recent advancements in technology have significantly improved the detection and measurement of antibodies. Techniques like mass spectrometry and next-generation sequencing are being explored for their potential to offer more detailed insights into antibody specificity and function. These innovations could lead to earlier diagnosis, more precise treatments, and improved patient outcomes.
Treatment Approaches
For Autoimmune Diseases
The treatment of autoimmune diseases aims to reduce inflammation, control the autoimmune response, and preserve organ function. Approaches include:
- Immunosuppressive drugs: To reduce immune system activity.
- Biologics: Targeted therapies that specifically block parts of the immune system involved in the disease.
- Physical therapy: To improve mobility and function in conditions like RA.
Lifestyle adjustments and supportive therapies also play a significant role in managing symptoms and enhancing quality of life.
Managing Alloantibodies in Transplants
Managing alloantibodies in transplant recipients involves pre-transplant screening and post-transplant monitoring. Strategies include:
- Immunosuppressive therapy adjustment: To prevent the formation of new alloantibodies.
- Plasmapheresis: To remove existing alloantibodies before transplantation.
- Immunomodulation: Using medications or treatments to decrease antibody production.
These approaches are crucial for preventing transplant rejection and extending the lifespan of the transplanted organ.
Emerging Therapies
Emerging therapies in the treatment of autoimmunity and alloantibody-related conditions focus on more specific and less toxic methods of modulating the immune system, such as:
- Monoclonal antibodies: Designed to target specific immune cells or proteins involved in the autoimmune process.
- Tolerance induction: Techniques aiming to retrain the immune system to recognize self-antigens as harmless.
- Gene editing: Potential future therapies could correct genetic predispositions to autoimmune diseases at the DNA level.
Ongoing research into these areas holds the promise of more effective and personalized treatment options for patients affected by these complex conditions.
Frequently Asked Questions
What are Alloantibodies?
Alloantibodies are antibodies that the immune system produces in response to and against foreign antigens from the same species. These are typically observed in scenarios like blood transfusions, where the immune system recognizes the donated blood as foreign and generates alloantibodies against it, or in organ transplants, impacting graft acceptance and longevity.
How do Autoantibodies Cause Disease?
Autoantibodies contribute to the development of autoimmune diseases by mistakenly targeting and attacking the body’s own cells, tissues, or organs. This misdirected immune response can lead to chronic inflammation, tissue damage, and dysfunction of the affected organs, manifesting as diseases like rheumatoid arthritis, lupus, and type 1 diabetes.
What is the Role of Alloantibodies in Transplantation?
In transplantation, alloantibodies can recognize and attack the transplanted organ or tissue as they would any foreign antigen. This immune response is a major cause of transplant rejection. Monitoring and managing levels of alloantibodies before and after transplantation are crucial for the success and longevity of the transplant.
How are Autoantibodies Detected?
Autoantibodies are detected using various laboratory tests, including ELISA (enzyme-linked immunosorbent assay), indirect immunofluorescence, and western blotting. These tests identify the presence and concentration of specific autoantibodies in the blood, aiding in the diagnosis of autoimmune diseases and monitoring disease activity.
Conclusion
The intricate dance between alloantibodies and autoantibodies within the human body underscores the immune system’s complexity and its pivotal role in health and disease. By differentiating between these two types of antibodies, medical science can better understand, diagnose, and treat a wide range of conditions, from autoimmune diseases to transplant rejection. This knowledge not only aids in the development of more effective treatments but also in the optimization of transplant procedures and the management of autoimmune conditions.
As research continues to unravel the mysteries of the immune system, the distinction between alloantibodies and autoantibodies remains a fundamental concept that bridges our understanding from basic immunology to clinical applications. The future promises further insights that will enhance our ability to harness the immune system’s power while mitigating its potential for self-harm, improving outcomes for patients worldwide.