The quest to combat microbial resistance has led to the development of various methods for testing the susceptibility of microorganisms to antibiotics. Among these methods, the Agar Well and Disc Diffusion techniques stand out as critical tools in the field of microbiology. These methods not only facilitate the identification of potent antimicrobial agents but also play a pivotal role in guiding the treatment strategies for infectious diseases.
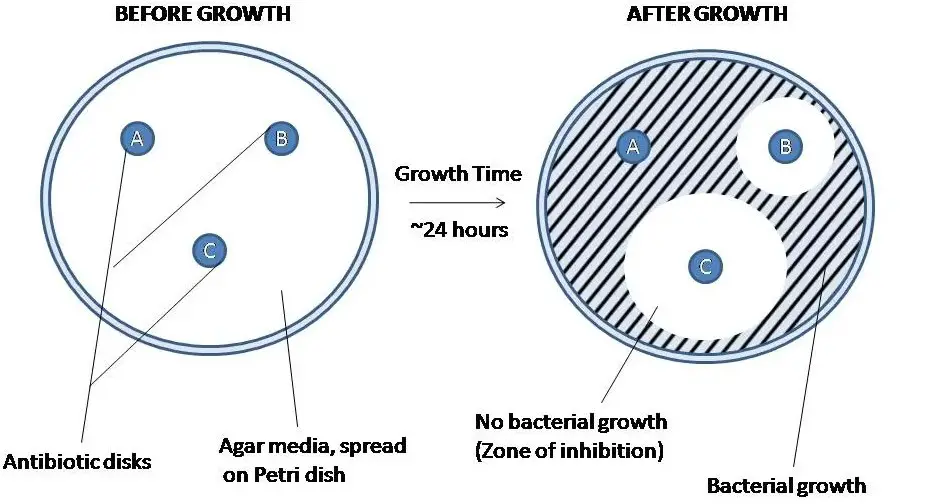
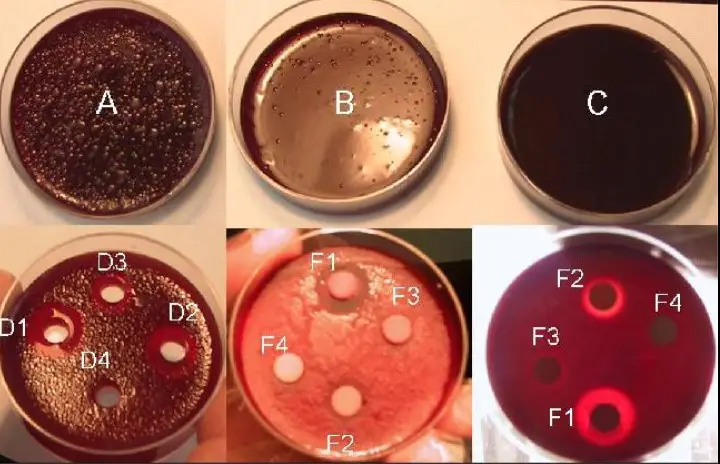
The difference between the Agar Well and Disc Diffusion methods lies in their approach to antimicrobial susceptibility testing. The Agar Well method involves creating wells in agar plates into which antibiotic solutions are added, while the Disc Diffusion method uses antibiotic-impregnated discs placed on the agar surface. Both methods measure the effectiveness of antibiotics by observing the inhibition zone around wells or discs, but they differ in procedure, application, and sensitivity.
Focusing on these differences offers insights into the suitability of each method for specific microbial analyses. The choice between Agar Well and Disc Diffusion methods depends on various factors including accuracy, cost, and the microbial species being tested. Understanding these methods provides a foundation for making informed decisions in microbial research and clinical diagnostics.
Agar Well Method
Overview
The Agar Well Method is a laboratory technique used in microbiology to test the effectiveness of antimicrobial agents against pathogens. This method is significant because it helps in identifying the most effective antibiotic for treating bacterial infections, thereby contributing to personalized medicine and combating antibiotic resistance.
Procedure
The procedure for the Agar Well method is straightforward and involves several key steps:
- Preparation of Agar Plates: Agar medium is poured into petri dishes and allowed to solidify.
- Inoculation: The surface of the agar is evenly inoculated with the bacterial strain of interest.
- Well Creation: Using a sterile borer, wells are created in the agar.
- Antibiotic Introduction: Different antibiotics are introduced into each well.
- Incubation: The plates are incubated at an appropriate temperature for a specific period.
- Observation: After incubation, the zones of inhibition around the wells are measured.
This method allows for the direct comparison of multiple antibiotics’ effectiveness against a specific bacterium.
Applications
The Agar Well Method is widely used in both clinical and research settings for various purposes:
- Determining Antibiotic Sensitivity: To identify which antibiotics are most effective against a particular bacterial strain.
- Research: In the study of microbial resistance and the development of new antimicrobial compounds.
- Quality Control: In the pharmaceutical industry, to ensure the potency of antibiotic products.
Its versatility makes it a valuable tool in the fight against infectious diseases.
Advantages
Several benefits make the Agar Well method favorable:
- Flexibility: It can test a wide range of antibiotics and concentrations.
- Quantitative Analysis: Provides clear, measurable zones of inhibition.
- Customizable: Can be adapted for specific microbes or antibiotics.
- Simplicity: Relatively easy to set up and interpret.
These advantages underscore the method’s utility in microbial susceptibility testing.
Limitations
Despite its benefits, the Agar Well method has limitations:
- Variability: Results can vary based on factors like agar thickness and well size.
- Subjectivity: Interpretation of zones can sometimes be subjective.
- Limited to Aerobic Bacteria: Primarily effective for bacteria that grow well on agar surfaces.
Awareness of these drawbacks is crucial for accurate interpretation of results.
Disc Diffusion Method
Overview
The Disc Diffusion Method, also known as the Kirby-Bauer method, plays a pivotal role in microbiology for assessing antibiotic sensitivity. This technique involves placing antibiotic-impregnated discs on an agar plate inoculated with a test organism. The ease of use and the visual clarity of the results have made it a standard method worldwide.
Procedure
The Disc Diffusion method follows a sequence of steps for its execution:
- Agar Preparation: Agar plates are prepared and inoculated with the bacterium to be tested.
- Placing Discs: Antibiotic discs are placed on the surface of the agar.
- Incubation: The plates are incubated, allowing the antibiotic to diffuse into the agar.
- Measuring Zones: The inhibition zones around the discs are measured after incubation.
This method provides a comparative measure of antibiotic effectiveness against specific bacteria.
Applications
The Disc Diffusion method is employed in various contexts:
- Clinical Diagnostics: To guide the treatment of bacterial infections by selecting effective antibiotics.
- Antibiotic Resistance Monitoring: For surveillance of resistance patterns in different geographical regions.
- Educational Purposes: As a teaching tool due to its simplicity and visual results.
Its application is critical for ensuring appropriate antibiotic usage.
Advantages
The Disc Diffusion method offers several key advantages:
- Standardized: Widely accepted and standardized, allowing for comparison across different laboratories.
- Cost-Effective: Relatively inexpensive compared to other antimicrobial susceptibility testing methods.
- User-Friendly: Easy to perform without the need for specialized equipment.
- Comprehensive: Capable of testing multiple antibiotics simultaneously.
These benefits make it an essential tool in microbiology laboratories.
Limitations
However, the Disc Diffusion method has its own set of limitations:
- Not Quantitative: Provides qualitative rather than quantitative data.
- Limited Scope: Not suitable for testing anaerobic bacteria or those requiring specialized growth conditions.
- Interpretation Challenges: Results can be influenced by factors such as agar depth and incubation conditions.
Comparative Analysis
Sensitivity and Accuracy
When comparing the sensitivity and accuracy of the Agar Well and Disc Diffusion methods, it’s crucial to understand the nuances that make each method suitable for different scenarios. Sensitivity refers to the method’s ability to detect minimal concentrations of antibiotics that inhibit bacterial growth, while accuracy involves the method’s precision in reflecting true antimicrobial activity.
- Agar Well Method: This method is often highlighted for its customizability in terms of antibiotic concentration, which can enhance sensitivity. However, variability in well size and agar depth may impact accuracy.
- Disc Diffusion Method: Known for its standardization, the Disc Diffusion method offers consistent results across different laboratories, making it highly accurate. Sensitivity might be slightly lower compared to Agar Well, as the antibiotic concentrations are fixed.
In contexts requiring high sensitivity to minute antibiotic concentrations, the Agar Well method may be preferred. Conversely, for broader, more standardized susceptibility testing, the Disc Diffusion method stands out.
Cost and Accessibility
Cost-effectiveness and accessibility are key considerations in the selection of an antimicrobial susceptibility testing method.
- Agar Well Method: Generally, this method can be more cost-effective for laboratories that already have the necessary equipment to create wells in agar plates. It’s also beneficial where specific antibiotic concentrations need to be tested, which might not be readily available in disc form. However, the requirement for additional steps, such as well creation, can increase labor costs.
- Disc Diffusion Method: The primary advantage here is the widespread availability of pre-impregnated antibiotic discs, which can lower initial setup costs and make this method more accessible to labs with limited resources. The ease of use and reduced preparation time also contribute to its cost-effectiveness.
In settings where budget constraints and resource availability are critical, the Disc Diffusion method might be the more accessible and economical choice.
Ease of Use
The ease of use and learning curve for both methods are important factors, especially in educational or resource-limited settings.
- Agar Well Method: This method requires a bit more technical skill, especially in creating uniform wells and accurately measuring antibiotic concentrations. The learning curve might be steeper for those new to laboratory techniques.
- Disc Diffusion Method: Due to its straightforwardness and the use of pre-prepared discs, the Disc Diffusion method is often considered easier for beginners to learn and execute. The process is more streamlined, with less room for error in preparation.
For laboratories with less experienced staff or those looking for a method that’s easy to teach and replicate, the Disc Diffusion method is generally more user-friendly.
Scope of Application
The scope and limitations of each method in various settings reveal their adaptability to different research and clinical needs.
- Agar Well Method: Excelling in research environments where specific antibiotic concentrations need to be tested or custom antibiotic combinations are required. Its flexibility makes it suitable for advanced antimicrobial studies but might be overkill for routine clinical testing.
- Disc Diffusion Method: Its standardization and ease of use make it ideal for routine clinical diagnostics. While it provides less flexibility in terms of antibiotic concentrations, it covers a wide range of commonly used antibiotics, making it practical for everyday use.
Choosing the right method depends largely on the specific requirements of the testing environment and the objectives of the antimicrobial susceptibility testing.
Choosing the Right Method
Factors to Consider
Several factors influence the choice between Agar Well and Disc Diffusion methods:
- Objective of Testing: Research vs. clinical diagnostics.
- Available Resources: Equipment, expertise, and financial considerations.
- Required Sensitivity and Specificity: Dependence on the nature of the bacterial infections and antibiotics in question.
- Ease of Procedure: Consideration of staff expertise and training.
- Turnaround Time: Urgency of the results.
Understanding these factors is essential for making an informed decision that aligns with the laboratory’s capabilities and the testing objectives.
Recommendations
Based on the above considerations, here are some recommendations for selecting the appropriate method:
- Research Applications: Opt for the Agar Well method when investigating new antibiotics or specific concentration effects due to its flexibility and sensitivity.
- Routine Clinical Testing: The Disc Diffusion method is recommended for its standardization, ease of use, and quick learning curve, making it suitable for fast-paced clinical environments.
- Limited Resources: For laboratories with constrained budgets or limited access to specialized equipment, the Disc Diffusion method offers a practical and economical option.
- Specialized Testing Needs: If testing requires customized antibiotic combinations or specific concentrations not available in disc form, the Agar Well method provides the necessary adaptability.
FAQs
What is Antimicrobial Susceptibility Testing?
Antimicrobial Susceptibility Testing (AST) is a laboratory procedure used to determine the efficacy of antibiotics against pathogenic microorganisms. By assessing the sensitivity or resistance of bacteria to various antimicrobial agents, AST guides the selection of effective treatments for infections, ensuring targeted and efficient therapeutic interventions.
How does the Agar Well method work?
The Agar Well method works by creating small wells in agar plates, into which antibiotic solutions are added. After incubation, the area around the wells is examined for bacterial growth inhibition. The presence of clear zones, or inhibition zones, indicates the effectiveness of the antibiotic against the bacteria tested, providing qualitative data on antimicrobial activity.
What makes the Disc Diffusion method unique?
The Disc Diffusion method is unique due to its simplicity and the visual ease of interpreting results. Antibiotic-impregnated discs are placed on an agar surface inoculated with the test organism. The antibiotic diffuses into the agar, and the effectiveness is measured by the diameter of the bacterial growth inhibition zone around each disc, offering a straightforward approach to determining microbial sensitivity.
Can these methods detect all types of antibiotic resistance?
While the Agar Well and Disc Diffusion methods are effective for assessing the susceptibility of a wide range of bacteria to antibiotics, they may not detect all types of antibiotic resistance. Certain mechanisms of resistance, particularly those affecting internal cellular targets or those involving efflux pumps, might require additional or more specialized tests for accurate detection.
Conclusion
The Agar Well and Disc Diffusion methods each offer unique advantages in the realm of antimicrobial susceptibility testing, serving as crucial tools in the ongoing fight against bacterial infections and resistance. While both methods aim to assess the effectiveness of antibiotics, their differences underscore the importance of selecting the right technique based on the specific needs of the study or clinical diagnosis.
Ultimately, the choice between these methods should be informed by factors such as sensitivity, specificity, cost, and the nature of the microbial organisms under investigation. As microbial resistance continues to evolve, the ongoing refinement and adaptation of these methodologies will remain central to the development of effective antimicrobial strategies, ensuring the continued efficacy of antibiotics in the treatment of infectious diseases.
