Hormones are the unsung heroes of the human body, coordinating a multitude of functions that keep us alive and thriving. Among these, Antidiuretic Hormone (ADH) and Aldosterone play pivotal roles in managing the delicate balance of fluids and electrolytes. Their functions, although intertwined, are distinct in maintaining homeostasis—a term referring to the body’s ability to maintain stable internal conditions.
ADH, produced by the pituitary gland, primarily governs water retention in the kidneys, thereby regulating blood pressure and volume. Aldosterone, secreted by the adrenal cortex, controls sodium and potassium levels, which in turn affect blood volume and pressure. While both hormones are critical for fluid balance, their mechanisms of action, triggers for release, and effects on the body differ significantly.
Understanding the differences between ADH and Aldosterone is crucial for comprehending how the body responds to changes in hydration and electrolyte levels. These differences not only highlight the body’s complexity but also shed light on how disorders related to these hormones can impact health. By exploring their distinct roles, we can appreciate the fine-tuning required for our body’s optimal functioning.
Hormones Explained
Hormones act as the body’s chemical messengers, playing a pivotal role in regulating physiological processes. Among these, Antidiuretic Hormone (ADH) and Aldosterone stand out for their critical functions in maintaining fluid and electrolyte balance.
ADH Overview
Definition and Production Site
ADH, also known as vasopressin, is a peptide hormone that regulates the body’s retention of water. It is synthesized in the hypothalamus and stored in the posterior pituitary gland for release into the bloodstream.
Main Functions
ADH’s primary function is to control the amount of water reabsorbed from the filtrate in the kidney tubules. This action directly influences blood volume and pressure, highlighting its role in homeostasis.
Aldosterone Overview
Definition and Production Site
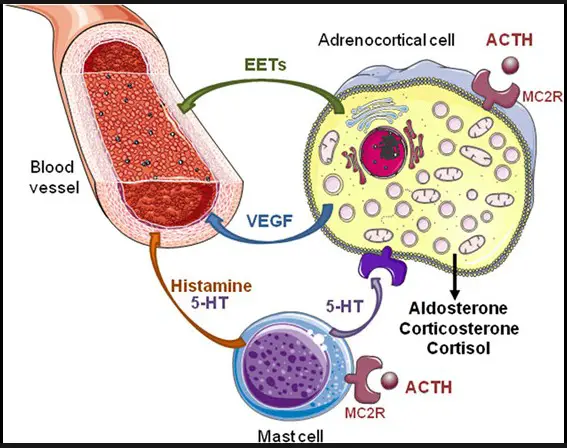
Aldosterone is a steroid hormone produced in the adrenal cortex. Part of the renin-angiotensin-aldosterone system (RAAS), it plays a critical role in regulating sodium and potassium levels in the body.
Main Functions
Aldosterone promotes the reabsorption of sodium and the excretion of potassium by the kidneys. This sodium retention leads to water retention, which increases blood volume and pressure, vital for cardiovascular health.
Key Functions
ADH in Action
Role in Water Balance
ADH ensures that the body conserves water when it’s needed, minimizing water loss through urine. This role is crucial in maintaining adequate blood volume and pressure.
Mechanism of Action in the Kidneys
- Detection of Low Blood Volume: The hypothalamus senses when blood volume is low and signals the pituitary gland to release ADH.
- Response in Kidneys: Upon reaching the kidneys, ADH makes the collecting ducts more permeable to water, leading to increased water reabsorption.
Aldosterone in Action
Role in Sodium and Potassium Balance
Aldosterone is key to managing sodium and potassium levels, essential elements in fluid balance and nerve functions.
Mechanism of Action in the Kidneys
- Sodium Reabsorption: Aldosterone signals the nephrons in the kidneys to reabsorb more sodium back into the bloodstream.
- Potassium Excretion: Simultaneously, it facilitates the excretion of potassium, maintaining the critical balance between these electrolytes.
Interplay and Regulation
ADH and Aldosterone Interaction
ADH and Aldosterone work together to maintain fluid and electrolyte balance, illustrating the body’s complex regulation system. Their actions complement each other, ensuring stable internal conditions.
Regulation Mechanisms
The body employs feedback mechanisms to regulate the levels of ADH and Aldosterone, adapting to changes in fluid and electrolyte status.
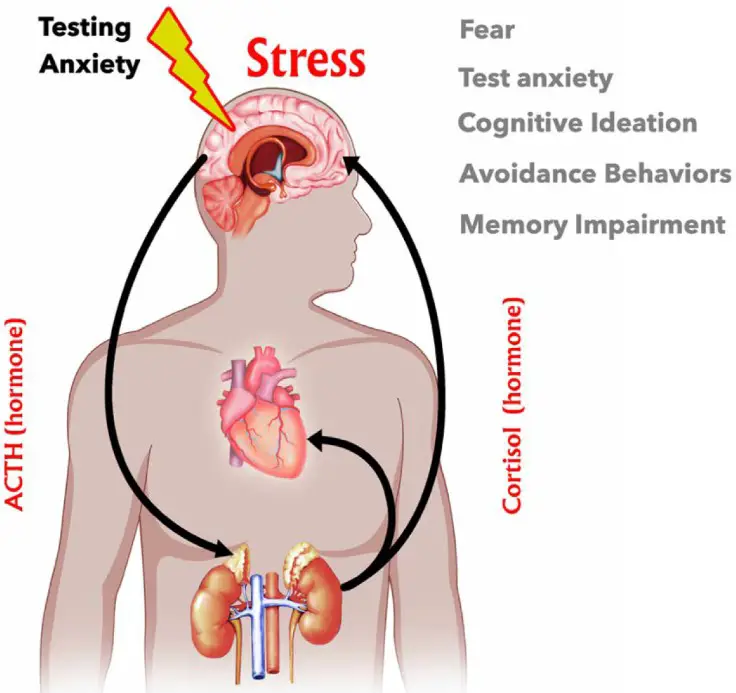
- For ADH: The primary triggers for its release are high blood osmolarity and low blood volume, sensed by osmoreceptors in the hypothalamus.
- For Aldosterone: The RAAS plays a crucial role, with renin release in response to low blood pressure initiating a cascade that increases Aldosterone production.
Physiological Effects
Effects of ADH
Impact on Blood Pressure and Volume
ADH plays a critical role in regulating blood volume and, consequently, blood pressure. By increasing water reabsorption in the kidneys, it ensures that the body conserves water, elevating blood volume and pressure when necessary. This mechanism is vital in preventing dehydration and maintaining circulatory stability.
Clinical Relevance: SIADH and Diabetes Insipidus
- SIADH (Syndrome of Inappropriate Antidiuretic Hormone): This condition involves excessive release of ADH, leading to water retention, diluted blood (hyponatremia), and potential swelling of tissues. Treatment focuses on limiting water intake and addressing the underlying cause.
- Diabetes Insipidus: In stark contrast to SIADH, Diabetes Insipidus is characterized by insufficient ADH, causing frequent urination and intense thirst. Management includes ADH replacement therapy to control symptoms.
Effects of Aldosterone
Impact on Blood Pressure and Volume
Aldosterone’s ability to regulate sodium reabsorption and potassium excretion directly influences blood volume and pressure. By promoting sodium retention, it indirectly causes water retention, thus increasing blood volume and pressure—a mechanism essential for cardiovascular health.
Clinical Relevance: Hyperaldosteronism and Addison’s Disease
- Hyperaldosteronism: This condition arises from excessive Aldosterone production, leading to high blood pressure, sodium retention, and potassium loss. Treatment may involve medications that block Aldosterone effects or surgery to remove an overactive adrenal gland.
- Addison’s Disease: Conversely, Addison’s Disease features insufficient Aldosterone (and cortisol), resulting in low blood pressure, dehydration, and electrolyte imbalances. Treatment typically includes hormone replacement therapy.
Comparative Analysis
Similarities Between ADH and Aldosterone
Both hormones are paramount in maintaining homeostasis, specifically in regulating fluid and electrolyte balance. Their actions ensure the body’s ability to adapt to changes in hydration status and electrolyte levels, maintaining stability in the internal environment.
Differences Summarized
- Production Sites: ADH is produced in the hypothalamus and released from the pituitary gland, whereas Aldosterone is secreted by the adrenal cortex.
- Triggers for Release: ADH release is primarily triggered by increased blood osmolarity or decreased blood volume. Aldosterone release is chiefly stimulated by the RAAS in response to low blood pressure and altered potassium levels.
- Primary Actions: ADH’s main action is to increase water reabsorption in the kidneys, while Aldosterone facilitates sodium reabsorption and potassium excretion.
Real-World Implications
Clinical Importance
Understanding the functions and regulation of ADH and Aldosterone is crucial in diagnosing and treating disorders related to these hormones. For instance, distinguishing between the symptoms of SIADH and Diabetes Insipidus or recognizing the signs of Hyperaldosteronism can lead to timely and effective treatment strategies.
Lifestyle and Diet
Daily choices regarding hydration and salt intake have significant impacts on ADH and Aldosterone levels, affecting fluid and electrolyte balance.
- Hydration: Adequate water intake can prevent the excessive release of ADH, maintaining proper hydration status and preventing conditions like hyponatremia.
- Salt Intake: High salt intake can suppress Aldosterone production, affecting blood pressure and potentially leading to hypertension if not balanced with other dietary and lifestyle factors.
Frequently Asked Questions
What triggers ADH release?
ADH release is primarily triggered by an increase in blood osmolarity, which signals the body’s need to conserve water. Other factors include low blood volume and stress, which also prompt the pituitary gland to release ADH, enhancing water reabsorption in the kidneys to adjust the blood’s osmolarity and volume.
How does Aldosterone affect blood pressure?
Aldosterone regulates blood pressure by controlling sodium and potassium levels in the blood. By promoting sodium reabsorption and potassium excretion in the kidneys, Aldosterone increases water retention, thus raising blood volume and pressure. This mechanism underscores its vital role in electrolyte balance and blood pressure regulation.
Can lifestyle choices affect ADH and Aldosterone levels?
Yes, lifestyle choices such as hydration, diet, and salt intake significantly influence ADH and Aldosterone levels. For instance, high salt intake can suppress Aldosterone production, while dehydration triggers ADH release to conserve water. Understanding these effects can help in making informed choices for maintaining fluid and electrolyte balance.
What are common disorders related to ADH and Aldosterone?
Disorders related to ADH include Diabetes Insipidus, characterized by insufficient ADH leading to excessive urination, and Syndrome of Inappropriate Antidiuretic Hormone (SIADH), where excessive ADH causes water retention. Aldosterone-related disorders include Addison’s Disease, with low Aldosterone levels, and Hyperaldosteronism, where excessive Aldosterone leads to high blood pressure.
Conclusion
The ballet of hormones within the human body is complex, with ADH and Aldosterone playing crucial roles in the intricate dance of fluid and electrolyte balance. Their differences underscore the body’s nuanced approach to maintaining homeostasis, revealing a fascinating aspect of human physiology. Understanding these mechanisms not only enriches our knowledge but also paves the way for addressing related health issues effectively.
The exploration of ADH and Aldosterone serves as a reminder of the elegance and precision with which our bodies operate. It highlights the importance of maintaining a healthy lifestyle to support these hormonal functions and the need for awareness regarding the symptoms and treatment of related disorders. As we uncover more about these hormones, we continue to marvel at the body’s ability to sustain life through a delicate, yet robust, balance.