The human body operates through a complex interplay of metabolic states, significantly influenced by our dietary intake. At the heart of this process lie two pivotal states: the absorptive and postabsorptive states. These phases orchestrate how our bodies process and utilize nutrients from the food we consume, playing a crucial role in maintaining our overall health and metabolic balance.
The difference between the absorptive and postabsorptive states lies in the body’s approach to handling glucose, fats, and proteins. During the absorptive state, the body metabolizes nutrients directly from the food we eat, primarily using glucose as its energy source and storing excess nutrients. Conversely, in the postabsorptive state, the body shifts to utilizing stored nutrients to maintain energy levels, tapping into fat reserves and other stored forms of energy.
Understanding these metabolic phases is not just academic; it has real-world implications for weight management, diabetes prevention, and overall metabolic health. By recognizing how our bodies switch between these states, we can better align our eating habits, exercise routines, and lifestyle choices to support our metabolic well-being, ultimately leading to a healthier life.
Metabolic States Overview
The human body undergoes various metabolic states throughout the day, primarily dictated by food intake and energy utilization. Understanding these states—absorptive and postabsorptive—offers insights into how the body manages nutrients and energy, crucial for maintaining health and preventing metabolic disorders.
Absorptive State
Definition
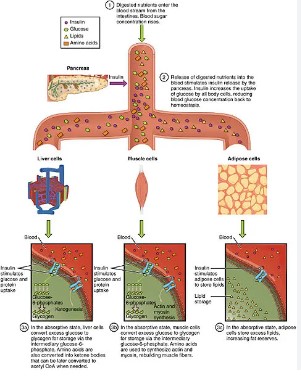
The absorptive state, also known as the fed state, occurs shortly after eating when the body digests food and absorbs nutrients through the intestinal mucosa into the bloodstream. This state is characterized by increased levels of glucose, amino acids, and lipids in the blood.
Time Frame Post-Eating
Typically, the absorptive state lasts for about 3 to 4 hours following a meal, during which the body prioritizes energy storage and nutrient utilization.
Key Hormones Involved
Insulin is the primary hormone active during this phase, facilitating glucose uptake by cells and promoting the synthesis of proteins, lipids, and glycogen.
Postabsorptive State
Definition
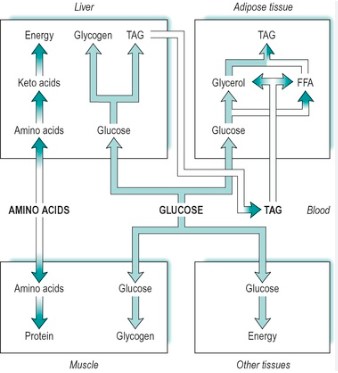
The postabsorptive state, or fasting state, commences once the body has finished processing and absorbing nutrients from a meal. During this phase, the body shifts its energy source from ingested food to stored reserves to maintain blood glucose levels and meet energy demands.
Time Frame Post-Absorption
This state can last until the next meal, often 12 hours or more, depending on the individual’s eating schedule and metabolic rate.
Key Hormones Involved
Glucagon, epinephrine, and norepinephrine are predominant during the postabsorptive state, triggering the mobilization of energy stores.
Energy Utilization
The body’s energy utilization shifts significantly between the absorptive and postabsorptive states, influenced largely by the availability of nutrients and the hormonal environment.
During Absorption
Glucose as Primary Energy Source
During the absorptive state, glucose serves as the main energy source for most body tissues, including the brain and muscles.
Role of Insulin
Insulin plays a critical role in facilitating glucose uptake by cells, thus supporting energy production. It also stimulates the synthesis of glycogen, fats, and proteins, ensuring that excess nutrients are efficiently stored for later use.
During Postabsorption
Energy Sources: Fatty Acids, Ketone Bodies
In the postabsorptive state, the body leans on fatty acids and ketone bodies derived from fat stores as primary energy sources. Glucose is preserved for organs that require it, such as the brain.
Role of Glucagon
Glucagon stimulates the breakdown of glycogen into glucose in the liver and the mobilization of fatty acids from adipose tissue, ensuring a continuous energy supply.
Hormonal Regulation
The transition between metabolic states and the corresponding energy utilization is tightly regulated by hormones, primarily insulin and glucagon, among others.
Insulin’s Role
Triggering Glucose Uptake
Insulin, secreted by the pancreas in response to elevated blood glucose levels, facilitates the uptake of glucose by cells, particularly muscle and adipose cells, for immediate use or storage.
Anabolic Processes
Insulin is also instrumental in promoting anabolic processes, such as the synthesis of glycogen, fats, and proteins, crucial for growth and repair.
Glucagon and Others
Stimulating Glycogenolysis and Gluconeogenesis
Glucagon opposes insulin’s actions by encouraging glycogenolysis (the breakdown of glycogen to glucose) and gluconeogenesis (the production of glucose from non-carbohydrate sources), vital during the postabsorptive state to maintain blood glucose levels.
Catabolic Processes
Besides glucagon, hormones like epinephrine and norepinephrine also contribute to catabolic processes, breaking down stored nutrients to sustain energy levels during periods of fasting or increased energy demands.

Impact on Body Systems
Our body is a complex machine, finely tuned to convert food into energy and rebuild itself. Let’s explore how different systems and practices affect our health and daily functioning.
Digestive System
Absorptive State Effects
The absorptive state happens right after you eat. Your digestive system breaks down food, absorbing nutrients and converting them into energy. During this time, glucose levels spike, and your body releases insulin to manage this surge, channeling glucose to cells for immediate use or storage.
Postabsorptive Adjustments
In contrast, the postabsorptive state occurs several hours after eating, signaling your body to switch from storing to utilizing energy. Your liver plays a hero, releasing stored glucose to maintain blood sugar levels. This balance is crucial for brain function and overall energy maintenance.
Muscular and Adipose Tissue
Fuel Storage and Mobilization
Muscles store glycogen, a quick energy source during sudden exertion, whereas adipose tissue (fat) stocks up on triglycerides, a more long-term energy reserve. Understanding how to manage these storage forms can optimize both health and physical performance.
Liver Functions
Central Role in Metabolism Transitions
The liver is a metabolic powerhouse, orchestrating the switch between the absorptive and postabsorptive states. It regulates blood sugar, detoxifies substances, and processes nutrients, acting as a control center for your body’s energy needs.
Health Implications
Weight Management
Managing weight revolves around balancing caloric intake with metabolic needs. Overeating or consuming high-calorie foods without corresponding physical activity can disrupt this balance, leading to weight gain and associated health risks.
Diabetes and Insulin Resistance
Diabetes and insulin resistance disrupt normal metabolic transitions, making it harder for the body to manage blood sugar levels. These conditions can stem from genetic factors, lifestyle choices, and dietary habits, highlighting the importance of diet and exercise in prevention and management.
Fasting and Feeding Cycles
Optimizing fasting and feeding cycles can enhance metabolic health, potentially reducing the risk of chronic diseases. Intermittent fasting, for example, alternates between periods of eating and fasting, improving insulin sensitivity and promoting better nutrient utilization.
Practical Applications
Nutritional Timing
Meal timing can significantly impact metabolic efficiency. Eating larger meals early in the day when metabolism is higher and tapering off towards the evening can promote better energy use and weight management.
- Breakfast: Start with a nutrient-rich meal to fuel your day.
- Lunch: Opt for a moderate meal to sustain energy.
- Dinner: Have a lighter meal to align with lower evening metabolism.
Exercise and Metabolism
Physical activity boosts metabolism, impacting both the absorptive and postabsorptive states. Exercise increases glucose uptake by muscles, reducing the need for insulin and improving blood sugar management.
- Before a meal: Can prime the body for better nutrient absorption.
- After a meal: Helps in quicker glucose utilization, preventing spikes in blood sugar.
Managing Blood Sugar
Maintaining stable blood sugar levels is essential for overall health, preventing spikes and crashes that can lead to fatigue and irritability. Here are simple strategies:
- Fiber-rich foods: Slow down glucose absorption, stabilizing blood sugar.
- Regular meals: Prevent large fluctuations in blood sugar levels.
- Physical activity: Increases insulin sensitivity, improving glucose management.

Frequently Asked Questions
What triggers the switch between absorptive and postabsorptive states?
The transition between absorptive and postabsorptive states is primarily regulated by the presence of nutrients in the bloodstream. Insulin plays a key role during the absorptive state by promoting glucose uptake and nutrient storage. As nutrient levels drop, insulin secretion decreases, and glucagon levels rise, signaling the body to enter the postabsorptive state and start mobilizing stored energy.
How does the absorptive state affect weight management?
During the absorptive state, the body’s focus on storing excess nutrients can impact weight management. Efficiently managing this state, such as by controlling portion sizes and choosing foods that promote a gradual release of glucose, can help prevent excessive calorie storage as fat, thereby supporting weight management efforts.
Can exercise influence metabolic states?
Yes, exercise can significantly influence metabolic states. Physical activity increases the body’s energy demands, encouraging the use of stored energy sources. During and after exercise, the body may increase its reliance on stored fats and glycogen, thereby affecting the duration and efficiency of the postabsorptive state and enhancing overall metabolic health.
What role does diet play in managing diabetes concerning these metabolic states?
Diet plays a critical role in managing diabetes by influencing how the body transitions between these metabolic states. A diet rich in fiber, healthy fats, and proteins can help stabilize blood glucose levels, promoting a more balanced transition between the absorptive and postabsorptive states. This can be particularly beneficial in managing insulin sensitivity and reducing the risk of diabetes-related complications.
Conclusion
The absorptive and postabsorptive states represent fundamental processes in our metabolic system, each playing a distinct role in how our bodies utilize and store nutrients. Recognizing the differences between these states not only enhances our understanding of metabolic health but also empowers us to make informed decisions about our diet and lifestyle choices. By aligning our eating habits and physical activity with these metabolic processes, we can better support our body’s energy needs and health objectives.
Ultimately, the knowledge of how these metabolic states function and affect our health is a powerful tool in our quest for a balanced and healthy life. As we continue to uncover the intricate details of these processes, we pave the way for more personalized and effective approaches to nutrition, exercise, and overall well-being.